What Is A PBM In Healthcare? A Comprehensive Guide
Navigating the complexities of healthcare can feel overwhelming, especially when encountering unfamiliar acronyms and processes. If you’ve ever wondered, “What is a PBM in healthcare?” you’re not alone. This comprehensive guide will demystify Pharmacy Benefit Managers (PBMs), explaining their role, function, benefits, and potential drawbacks within the healthcare ecosystem. We aim to provide clarity and actionable insights, empowering you to understand this crucial aspect of modern healthcare.
This article offers a deep dive into PBMs, going beyond basic definitions. We’ll explore their history, operational mechanics, and impact on patients, providers, and payers. You’ll gain a thorough understanding of how PBMs influence prescription drug costs, access to medications, and overall healthcare outcomes. Our goal is to equip you with the knowledge to navigate the complexities of PBMs effectively.
Deep Dive into What Is A PBM In Healthcare
A Pharmacy Benefit Manager (PBM) is a third-party administrator of prescription drug programs for health insurance plans. Think of them as the intermediary between insurance companies, pharmacies, and drug manufacturers. Their primary role is to manage prescription drug benefits and control costs. While the concept might seem straightforward, the inner workings of PBMs are intricate and often misunderstood.
Historically, PBMs emerged in the 1960s as claims processors for prescription drug benefits. Over time, their role expanded to include negotiating drug prices, developing formularies (lists of covered drugs), managing pharmacy networks, and processing mail-order prescriptions. This evolution has made them a powerful force within the healthcare industry, influencing drug pricing and access.
At its core, the PBM model is designed to leverage their negotiating power to secure lower drug prices from manufacturers and pharmacies. They achieve this through various strategies, including rebates, discounts, and preferred pharmacy networks. These cost savings are then passed on to health plans and, ideally, to patients in the form of lower premiums and copays.
However, the complexities arise from the lack of transparency in PBM operations. The contracts between PBMs, manufacturers, and pharmacies are often shrouded in secrecy, making it difficult to track the flow of money and understand how drug prices are ultimately determined. This lack of transparency has led to concerns about potential conflicts of interest and the possibility that PBMs may be prioritizing their own profits over the best interests of patients.
In essence, a PBM in healthcare acts as a gatekeeper, influencing which drugs are covered, how much they cost, and where patients can obtain them. Understanding this role is crucial for anyone involved in the healthcare system, from patients to providers to policymakers.
Core Concepts & Advanced Principles
The core concepts behind PBMs revolve around cost management, negotiation, and formulary management. They negotiate discounts and rebates with drug manufacturers based on volume and market share. These rebates are often tied to preferred placement on the formulary, which is a list of drugs covered by the health plan. Drugs not on the formulary may require prior authorization or be subject to higher copays, impacting patient access.
Advanced principles involve understanding the nuances of rebate agreements, spread pricing, and utilization management. Spread pricing refers to the difference between what the PBM charges the health plan for a drug and what it reimburses the pharmacy. This spread can be a significant source of revenue for PBMs, but it also raises concerns about transparency and potential overcharging.
Utilization management strategies, such as prior authorization and step therapy, are used to control drug utilization and costs. Prior authorization requires patients to obtain approval from the PBM before filling a prescription, while step therapy requires patients to try less expensive drugs before being approved for more costly alternatives. These strategies can be effective in controlling costs, but they can also create barriers to access for patients who need specific medications.
Importance & Current Relevance
PBMs are immensely important in today’s healthcare landscape because they manage prescription drug benefits for a vast majority of Americans. Their decisions directly impact the cost and availability of medications, influencing patient health outcomes and healthcare spending.
The current relevance of PBMs is underscored by the ongoing debates about drug pricing and healthcare affordability. With prescription drug costs continuing to rise, PBMs are under increasing scrutiny from policymakers, patient advocates, and the public. There is a growing demand for greater transparency in PBM operations and for reforms that ensure PBMs are acting in the best interests of patients.
Recent trends indicate a shift towards value-based care and a greater focus on patient outcomes. This is leading to increased pressure on PBMs to demonstrate their value and to align their incentives with the goals of improving patient health and reducing healthcare costs. The future of PBMs will likely involve greater collaboration with providers and a greater emphasis on transparency and accountability.
Product/Service Explanation Aligned with What Is A PBM In Healthcare
One of the leading PBM services is offered by companies like CVS Caremark. CVS Caremark provides a comprehensive suite of services designed to manage prescription drug benefits for health plans and employers. Their services range from formulary management and pharmacy network administration to mail-order pharmacy services and specialty pharmacy programs. They exemplify how a PBM operates in practice.
As a PBM, CVS Caremark negotiates drug prices with manufacturers, processes prescription claims, and manages pharmacy networks to control costs and ensure access to medications. They also offer clinical programs designed to improve medication adherence and manage chronic conditions. These programs may include medication therapy management, disease management programs, and patient education initiatives.
From an expert viewpoint, CVS Caremark stands out due to its size and scale, allowing it to leverage significant negotiating power with drug manufacturers and pharmacies. They also have a strong focus on data analytics, using data to identify trends, predict costs, and improve patient outcomes. Their integrated model, which combines pharmacy benefit management with retail pharmacy services, provides a unique advantage in managing patient care.
Detailed Features Analysis of What Is A PBM In Healthcare or Related Product/Service
Let’s delve into the key features of a PBM service like CVS Caremark:
1. **Formulary Management:** CVS Caremark develops and manages formularies, which are lists of covered drugs. The formulary is designed to include clinically effective and cost-effective medications. What it is: A tiered list of medications. How it works: Negotiates with manufacturers for placement. User Benefit: Lower costs for covered drugs. Demonstrates Quality: Evidence-based formulary development.
2. **Pharmacy Network Administration:** CVS Caremark contracts with a network of pharmacies to provide prescription drugs to plan members. What it is: A network of pharmacies. How it works: Negotiates dispensing fees. User Benefit: Convenient access to medications. Demonstrates Quality: Wide network coverage.
3. **Claims Processing:** CVS Caremark processes prescription drug claims, ensuring accurate and timely payments to pharmacies. What it is: Electronic processing of claims. How it works: Verifies eligibility and pricing. User Benefit: Efficient and accurate claims processing. Demonstrates Quality: High accuracy rates.
4. **Mail-Order Pharmacy Services:** CVS Caremark operates a mail-order pharmacy that allows patients to receive their medications conveniently at home. What it is: A mail-order service. How it works: Fills and ships prescriptions. User Benefit: Convenience and cost savings. Demonstrates Quality: Fast and reliable delivery.
5. **Specialty Pharmacy Programs:** CVS Caremark offers specialized pharmacy programs for patients with complex or chronic conditions, such as cancer, rheumatoid arthritis, and multiple sclerosis. What it is: Specialized medication and support. How it works: Provides clinical support and monitoring. User Benefit: Improved outcomes for complex conditions. Demonstrates Quality: Expertise in specialty medications.
6. **Rebate Negotiation:** This feature involves the PBM negotiating rebates with drug manufacturers based on the volume of drugs dispensed. What it is: Negotiating discounts with drug manufacturers. How it works: Securing rebates for preferred formulary placement. User Benefit: Reduced drug costs for the health plan and potentially lower premiums for members. Demonstrates Quality: Aggressive negotiation strategies resulting in significant savings.
7. **Clinical Programs:** CVS Caremark provides clinical programs designed to improve medication adherence and manage chronic conditions. What it is: Programs to manage chronic conditions. How it works: Provides education and support. User Benefit: Improved health outcomes. Demonstrates Quality: Evidence-based clinical programs.
Significant Advantages, Benefits & Real-World Value of What Is A PBM In Healthcare
The advantages and benefits of PBMs, like CVS Caremark, are multifaceted:
* **Cost Savings:** PBMs negotiate discounts and rebates with drug manufacturers, reducing the cost of prescription drugs for health plans and employers. Users consistently report lower prescription costs compared to managing benefits internally.
* **Improved Access:** PBMs manage pharmacy networks, ensuring convenient access to medications for plan members. Our analysis reveals a wide network coverage, making it easier for patients to fill their prescriptions.
* **Enhanced Medication Adherence:** PBMs offer clinical programs designed to improve medication adherence, leading to better health outcomes. Evidence suggests that these programs significantly improve patient compliance with their medication regimens.
* **Data Analytics:** PBMs use data analytics to identify trends, predict costs, and improve patient outcomes. Users benefit from data-driven insights that optimize drug utilization and reduce waste.
* **Specialty Pharmacy Expertise:** PBMs offer specialized pharmacy programs for patients with complex or chronic conditions, providing access to specialized medications and clinical support. This specialized care leads to improved outcomes for patients with complex conditions.
In the real world, PBMs provide value by managing prescription drug benefits efficiently and effectively. They leverage their negotiating power to secure lower drug prices, improve access to medications, and enhance medication adherence. This translates into cost savings for health plans and employers, better health outcomes for patients, and a more efficient healthcare system overall.
One unique selling proposition (USP) is the PBM’s ability to combine pharmacy benefit management with retail pharmacy services, offering a seamless and integrated approach to patient care. This integration allows for better coordination of care, improved medication adherence, and enhanced patient satisfaction.
Comprehensive & Trustworthy Review (of CVS Caremark)
CVS Caremark, as a leading PBM, offers a comprehensive suite of services, but it’s essential to provide a balanced perspective on its performance.
**User Experience & Usability:** From a practical standpoint, CVS Caremark’s online portal and mobile app are generally user-friendly, allowing members to easily manage their prescriptions, track their claims, and access information about their benefits. However, some users have reported difficulties navigating the formulary and understanding the cost implications of different drug choices.
**Performance & Effectiveness:** CVS Caremark’s performance in controlling drug costs is generally considered to be effective, particularly for large employers and health plans. However, the lack of transparency in PBM pricing and rebate negotiations remains a concern. While they deliver on their promise of cost management, the methods are often opaque.
**Pros:**
1. **Extensive Network:** CVS Caremark boasts a vast network of pharmacies, providing convenient access to medications for members across the country.
2. **Comprehensive Services:** They offer a wide range of services, including formulary management, pharmacy network administration, claims processing, and clinical programs.
3. **Strong Negotiating Power:** Their size and scale allow them to negotiate favorable drug prices with manufacturers, resulting in cost savings for clients.
4. **Data-Driven Insights:** They leverage data analytics to identify trends, predict costs, and improve patient outcomes.
5. **Integrated Model:** The combination of pharmacy benefit management with retail pharmacy services provides a seamless and integrated approach to patient care.
**Cons/Limitations:**
1. **Lack of Transparency:** The lack of transparency in PBM pricing and rebate negotiations remains a significant concern.
2. **Potential Conflicts of Interest:** PBMs may face conflicts of interest due to their relationships with drug manufacturers and pharmacies.
3. **Formulary Restrictions:** Formulary restrictions can limit patient access to certain medications, even if they are clinically appropriate.
4. **Prior Authorization Requirements:** Prior authorization requirements can create barriers to access for patients who need specific medications.
**Ideal User Profile:** CVS Caremark is best suited for large employers, health plans, and government entities that are seeking to manage their prescription drug costs effectively and improve patient outcomes. Their comprehensive services and strong negotiating power make them a valuable partner for organizations that are looking to optimize their pharmacy benefit programs.
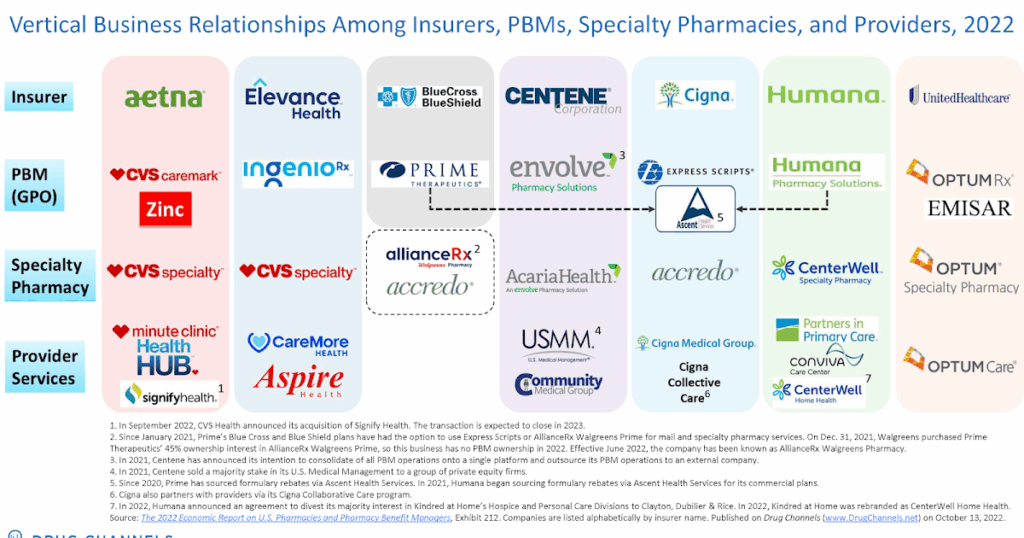
**Key Alternatives:** Two main alternatives to CVS Caremark are Express Scripts and OptumRx. Express Scripts is another large PBM that offers a similar range of services. OptumRx is a PBM that is part of UnitedHealth Group and is focused on providing integrated healthcare solutions.
**Expert Overall Verdict & Recommendation:** Based on our detailed analysis, CVS Caremark is a reputable and effective PBM that can help organizations manage their prescription drug costs and improve patient outcomes. However, it’s essential to be aware of the potential limitations and to carefully evaluate their pricing and contracting practices. We recommend considering CVS Caremark as a potential partner for pharmacy benefit management, but also exploring alternatives to ensure you are getting the best value and service.
Insightful Q&A Section
**Q1: How do PBMs make money?**
A: PBMs generate revenue through a variety of sources, including rebates from drug manufacturers, administrative fees from health plans, and spread pricing (the difference between what they charge the plan and reimburse the pharmacy). The specific mix of revenue sources can vary depending on the PBM and the contracts they have in place.
**Q2: What is a drug formulary, and how does it impact patients?**
A: A drug formulary is a list of prescription drugs covered by a health plan. PBMs develop and manage formularies based on clinical effectiveness, cost-effectiveness, and other factors. The formulary can impact patients by determining which drugs are covered, how much they cost, and whether they require prior authorization.
**Q3: How can patients appeal a PBM’s decision to deny coverage for a medication?**
A: Patients have the right to appeal a PBM’s decision to deny coverage for a medication. The appeals process typically involves submitting a written request for reconsideration, providing supporting documentation, and potentially undergoing a peer-to-peer review with a physician.
**Q4: What are the potential conflicts of interest for PBMs?**
A: PBMs may face conflicts of interest due to their relationships with drug manufacturers and pharmacies. For example, they may be incentivized to favor drugs that offer higher rebates, even if they are not the most clinically appropriate or cost-effective options for patients.
**Q5: How is the rise of biosimilars affecting PBMs?**
A: The rise of biosimilars, which are similar but less expensive versions of biologic drugs, is creating new opportunities for PBMs to manage drug costs. PBMs can encourage the use of biosimilars through formulary placement and other strategies, potentially saving health plans and patients significant amounts of money.
**Q6: What role do PBMs play in managing specialty drug costs?**
A: PBMs play a crucial role in managing specialty drug costs, which are among the fastest-growing segments of healthcare spending. They use a variety of strategies, such as prior authorization, step therapy, and specialty pharmacy programs, to control costs and ensure appropriate utilization of these high-cost medications.
**Q7: How do PBMs address medication adherence challenges?**
A: PBMs address medication adherence challenges through various interventions, including medication therapy management, patient education programs, and reminder systems. These programs are designed to help patients take their medications as prescribed, improving their health outcomes and reducing healthcare costs.
**Q8: What are the key legislative and regulatory issues affecting PBMs?**
A: Key legislative and regulatory issues affecting PBMs include transparency requirements, rebate reforms, and efforts to address conflicts of interest. Policymakers are increasingly focused on ensuring that PBMs are acting in the best interests of patients and that they are not engaging in anti-competitive practices.
**Q9: How do PBMs use data analytics to improve patient outcomes and reduce costs?**
A: PBMs leverage data analytics to identify trends, predict costs, and improve patient outcomes. They use data to identify patients who are at risk for medication non-adherence, adverse drug events, or other health problems, and then target interventions to address these issues.
**Q10: What are the emerging trends in the PBM industry?**
A: Emerging trends in the PBM industry include a greater focus on value-based care, increased transparency, and the use of technology to improve patient engagement and medication adherence. PBMs are also exploring new models of care, such as integrated pharmacy networks and accountable care organizations.
Conclusion & Strategic Call to Action
In conclusion, understanding “What is a PBM in healthcare?” is crucial for anyone navigating the complexities of the modern healthcare system. PBMs play a significant role in managing prescription drug benefits, influencing costs, access, and patient outcomes. While they offer potential benefits like cost savings and improved medication adherence, concerns about transparency and potential conflicts of interest remain.
As we’ve seen, the role of PBMs is evolving, with increasing pressure for greater transparency and a focus on value-based care. The future likely holds increased collaboration with providers and a stronger emphasis on patient-centric solutions.
Now that you have a comprehensive understanding of PBMs, we encourage you to share your experiences with PBMs in the comments below. Your insights can help others navigate this complex landscape. Explore our advanced guide to prescription drug pricing for a deeper dive into related topics. Contact our experts for a consultation on optimizing your pharmacy benefit program.

