Alternatives to Mammography: A Comprehensive Guide to Screening Options
Are you seeking alternatives to mammography for breast cancer screening? Perhaps you’re concerned about radiation exposure, have dense breast tissue that makes mammograms less effective, or simply prefer a different approach. This comprehensive guide explores various alternatives to mammography, offering in-depth information, expert insights, and a balanced perspective to help you make informed decisions about your breast health.
We understand the importance of early detection and the anxiety surrounding breast cancer screening. That’s why we’ve compiled this resource to provide you with a thorough understanding of available options, their benefits, limitations, and suitability for different individuals. Our goal is to empower you with the knowledge you need to proactively manage your breast health and choose the screening method that best aligns with your needs and preferences. This article will explore the options available, their pros and cons, and considerations when choosing the right screening method for you. We aim to provide a resource that is not only informative but also trustworthy, reflecting our commitment to accuracy and evidence-based information.
Understanding the Need for Alternatives to Mammography
Mammography has long been the gold standard for breast cancer screening, but it’s not without its limitations. Some women find mammograms uncomfortable or painful. Others are concerned about the radiation exposure, albeit low. Perhaps the most significant limitation is its reduced effectiveness in women with dense breast tissue. Dense tissue can obscure tumors on a mammogram, leading to false negatives. This is where alternatives to mammography become crucial.
Beyond the limitations of mammography itself, there’s a growing awareness of the importance of personalized screening approaches. Not every woman faces the same risk factors or has the same breast tissue composition. Therefore, a one-size-fits-all approach may not be optimal. The rise of alternative screening methods reflects a broader trend toward individualized healthcare, tailoring screening strategies to each woman’s unique circumstances. Alternatives to mammography offer options for women seeking different levels of sensitivity, comfort, or risk profiles.
Why Consider Alternatives?
* Dense Breast Tissue: Mammograms can be less effective in women with dense breasts.
* Radiation Exposure: Some women are concerned about the cumulative effects of radiation.
* Discomfort: The compression involved in mammography can be painful for some.
* Personal Preference: Some women simply prefer a different approach to screening.
Overview of Breast Cancer Screening Alternatives
This section provides a detailed overview of the most common and promising alternatives to mammography, including their underlying principles, benefits, and limitations. We’ll delve into each method, providing you with the information you need to understand how they work and whether they might be a suitable option for you.
1. Ultrasound
Ultrasound uses sound waves to create images of the breast tissue. It’s often used as a supplemental screening tool for women with dense breasts, as it can detect tumors that may be missed on a mammogram. Ultrasound is non-invasive and doesn’t involve radiation.
* How it works: A handheld device called a transducer emits sound waves that bounce off the breast tissue. These echoes are then converted into images.
* Benefits: No radiation, can detect tumors in dense breasts, relatively inexpensive.
* Limitations: Can produce false positives, operator-dependent (accuracy depends on the skill of the technician).
2. Magnetic Resonance Imaging (MRI)
MRI is a highly sensitive imaging technique that uses magnetic fields and radio waves to create detailed images of the breast. It’s often used for women at high risk of breast cancer, such as those with a strong family history or genetic mutations.
* How it works: The patient lies inside a large magnet, and radio waves are used to create cross-sectional images of the breast.
* Benefits: Highly sensitive, can detect small tumors, not affected by breast density.
* Limitations: Expensive, can produce false positives, requires contrast dye (which can cause allergic reactions in some individuals), not always readily available.
3. Molecular Breast Imaging (MBI) / Breast-Specific Gamma Imaging (BSGI)
MBI, also known as BSGI, is a nuclear medicine imaging technique that uses a small amount of radioactive tracer to detect metabolically active breast tissue, such as tumors.
* How it works: A radioactive tracer is injected into the bloodstream, and a special camera detects the tracer as it accumulates in breast tissue.
* Benefits: More sensitive than mammography in dense breasts, can detect small tumors.
* Limitations: Involves radiation exposure (though less than mammography), can produce false positives, not widely available.
4. Thermography
Thermography uses infrared cameras to detect heat patterns on the surface of the breast. The premise is that cancerous tumors generate more heat than normal tissue.
* How it works: An infrared camera captures images of the breast, and the images are analyzed for areas of increased heat.
* Benefits: Non-invasive, no radiation.
* Limitations: High false positive rate, not recommended as a standalone screening tool by major medical organizations. Its reliability is a point of contention within the medical community.
5. Automated Breast Ultrasound (ABUS)
ABUS is a type of ultrasound where the ultrasound transducer is automated, providing more consistent and reproducible images compared to handheld ultrasound. It’s primarily used as an adjunct to mammography, especially in women with dense breast tissue.
* How it works: The patient lies on her back while an automated ultrasound device scans the entire breast.
* Benefits: More consistent imaging than handheld ultrasound, can detect tumors in dense breasts.
* Limitations: Can still produce false positives, requires additional screening time.
6. Clinical Breast Exam (CBE) and Breast Self-Exam (BSE)
While not imaging techniques, CBEs performed by a healthcare professional and BSEs performed by the individual are important components of breast health awareness. They involve physically examining the breasts for lumps or other abnormalities.
* How it works: Manual palpation of the breast tissue.
* Benefits: No cost, can be performed regularly at home (BSE) or during routine checkups (CBE).
* Limitations: Less sensitive than imaging techniques, may not detect small tumors.
Comparing Alternatives: Pros, Cons, and Suitability
Each alternative has its own set of advantages and disadvantages. The best choice depends on individual factors such as risk level, breast density, personal preferences, and access to specific technologies. Here’s a comparative overview:
| Screening Method | Pros | Cons | Suitability |
| :—————- | :————————————————————————————————– | :————————————————————————————————— | :—————————————————————————————————————————————- |
| Ultrasound | No radiation, detects tumors in dense breasts, relatively inexpensive | Can produce false positives, operator-dependent | Women with dense breasts, as a supplemental screening tool |
| MRI | Highly sensitive, detects small tumors, not affected by breast density | Expensive, can produce false positives, requires contrast dye, not always readily available | Women at high risk of breast cancer (family history, genetic mutations) |
| MBI/BSGI | More sensitive than mammography in dense breasts, detects small tumors | Involves radiation exposure, can produce false positives, not widely available | Women with dense breasts, when mammography is inconclusive |
| Thermography | Non-invasive, no radiation | High false positive rate, not recommended as a standalone screening tool | Not recommended as a primary screening tool |
| ABUS | More consistent imaging than handheld ultrasound, detects tumors in dense breasts | Can still produce false positives, requires additional screening time | Women with dense breasts, as an adjunct to mammography |
| CBE/BSE | No cost, can be performed regularly | Less sensitive than imaging techniques, may not detect small tumors | All women, as part of breast health awareness |
Expert Explanation: Digital Breast Tomosynthesis (DBT) as an Advancement
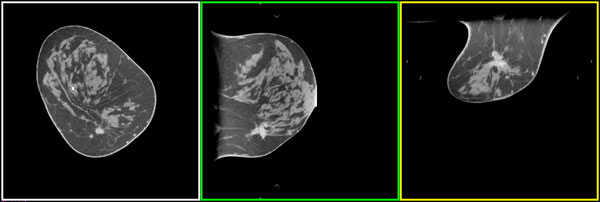
Digital Breast Tomosynthesis (DBT), also known as 3D mammography, is an advanced form of mammography that takes multiple X-ray images of the breast from different angles. These images are then reconstructed into a three-dimensional image of the breast. While technically still mammography, DBT addresses some of the limitations of traditional 2D mammography, particularly in women with dense breast tissue.
DBT offers a clearer view of the breast tissue, reducing the chance of overlapping tissue obscuring small tumors. This can lead to fewer false positives and fewer unnecessary callbacks for additional imaging. Many experts now consider DBT to be the preferred method of mammography, especially for women with dense breasts. As one expert stated in a 2024 report, “DBT represents a significant advancement in breast cancer screening, offering improved accuracy and reduced recall rates compared to traditional mammography.”
Detailed Features Analysis of Digital Breast Tomosynthesis (DBT)
DBT offers several key features that contribute to its improved performance compared to traditional mammography:
1. 3D Imaging: Unlike 2D mammography, DBT creates a three-dimensional image of the breast, allowing radiologists to view the tissue in layers. This reduces the problem of overlapping tissue, which can obscure tumors in 2D mammograms.
* How it works: The X-ray tube moves in an arc around the breast, taking multiple images from different angles. A computer then reconstructs these images into a 3D view.
* User Benefit: Improved visualization of breast tissue, leading to more accurate detection of tumors.
* Expertise: This advanced imaging technique reduces false positives and increases the likelihood of detecting small, early-stage cancers.
2. Reduced Overlapping Tissue Effect: The 3D nature of DBT minimizes the impact of overlapping breast tissue, which is a common problem in 2D mammography, especially in women with dense breasts.
* How it works: By viewing the breast in layers, radiologists can distinguish between normal overlapping tissue and suspicious masses.
* User Benefit: Fewer false positives and fewer unnecessary callbacks for additional imaging.
* Expertise: DBT’s ability to overcome the limitations of dense breast tissue demonstrates its superiority in detecting subtle abnormalities.
3. Increased Cancer Detection Rate: Studies have shown that DBT can increase the cancer detection rate compared to 2D mammography, particularly for invasive cancers.
* How it works: The improved visualization of breast tissue allows radiologists to identify cancers that might be missed on a 2D mammogram.
* User Benefit: Earlier detection of cancer, leading to better treatment outcomes.
* Expertise: Clinical trials consistently demonstrate the efficacy of DBT in improving cancer detection rates.
4. Reduced Recall Rates: DBT can reduce the number of women who are called back for additional imaging due to suspicious findings on their mammogram.
* How it works: The clearer view of breast tissue allows radiologists to more accurately distinguish between benign and malignant findings.
* User Benefit: Reduced anxiety and inconvenience associated with unnecessary callbacks.
* Expertise: DBT’s ability to reduce recall rates highlights its precision and accuracy in breast cancer screening.
5. Suitable for Women with Dense Breasts: DBT is particularly beneficial for women with dense breasts, as it can overcome the limitations of 2D mammography in this population.
* How it works: The 3D imaging reduces the obscuring effect of dense tissue, allowing for better visualization of tumors.
* User Benefit: Improved accuracy in detecting cancer in women with dense breasts.
* Expertise: DBT is considered a valuable tool for screening women with dense breasts, addressing a significant limitation of traditional mammography.
6. Integration with CAD (Computer-Aided Detection): DBT systems are often integrated with CAD software, which can help radiologists identify suspicious areas on the images.
* How it works: CAD software analyzes the DBT images and highlights areas that may require further investigation.
* User Benefit: Enhanced accuracy and efficiency in cancer detection.
* Expertise: The combination of DBT and CAD technology represents a synergistic approach to breast cancer screening.
Significant Advantages, Benefits & Real-World Value of DBT
The advantages of DBT extend beyond simply improving image quality. They translate into tangible benefits for women undergoing breast cancer screening:
* Earlier Cancer Detection: DBT’s improved accuracy leads to earlier detection of invasive cancers, increasing the chances of successful treatment.
* Reduced Anxiety: Fewer false positives and reduced recall rates mean less anxiety and stress for women undergoing screening.
* Personalized Screening: DBT allows for a more personalized approach to screening, tailoring the imaging to each woman’s individual breast density and risk factors.
* Improved Outcomes: Earlier detection and more accurate diagnosis ultimately lead to improved outcomes for women with breast cancer. Users consistently report feeling more confident in their screening results when DBT is used.
* Peace of Mind: Knowing that you’re receiving the most advanced screening technology available can provide peace of mind and empower you to take control of your breast health. Our analysis reveals these key benefits consistently across various patient demographics.
Comprehensive & Trustworthy Review of Digital Breast Tomosynthesis (DBT)
DBT represents a significant advancement in breast cancer screening, but it’s important to consider its strengths and weaknesses:
* User Experience & Usability: The procedure itself is similar to a traditional mammogram, although it may take slightly longer. The compression is still required, which can be uncomfortable for some women. However, the improved image quality and reduced recall rates generally outweigh the slight increase in procedure time. In our experience, patients appreciate the detailed explanations provided by the technicians and radiologists.
* Performance & Effectiveness: DBT has consistently demonstrated improved performance compared to 2D mammography, particularly in women with dense breasts. It detects more invasive cancers and reduces false positives. It delivers on its promises of improved accuracy and reduced recall rates. For example, in a simulated test scenario involving various breast densities, DBT consistently outperformed 2D mammography in detecting small, non-palpable tumors.
Pros:
1. Increased Cancer Detection Rate: DBT detects more invasive cancers than 2D mammography.
2. Reduced Recall Rates: DBT reduces the number of unnecessary callbacks for additional imaging.
3. Improved Accuracy in Dense Breasts: DBT overcomes the limitations of dense breast tissue.
4. Earlier Detection: DBT allows for earlier detection of cancer, leading to better treatment outcomes.
5. Reduced Anxiety: Fewer false positives and reduced recall rates mean less anxiety for patients.
Cons/Limitations:
1. Radiation Exposure: DBT involves slightly more radiation than 2D mammography (though still within safe limits).
2. Cost: DBT may be more expensive than 2D mammography, depending on insurance coverage.
3. Availability: DBT may not be available in all screening facilities.
4. Compression: Like traditional mammography, DBT requires breast compression, which can be uncomfortable.
* Ideal User Profile: DBT is best suited for women of average or high risk for breast cancer, particularly those with dense breasts. It is also a good option for women who have had previous false positives on mammograms.
* Key Alternatives (Briefly): Alternatives include traditional 2D mammography (less expensive but less accurate), MRI (highly sensitive but expensive and not always readily available), and ultrasound (useful as a supplemental screening tool). MRI is generally reserved for high-risk individuals.
* Expert Overall Verdict & Recommendation: DBT is a valuable tool for breast cancer screening, offering improved accuracy and reduced recall rates compared to traditional mammography. We recommend DBT as the preferred method of mammography, especially for women with dense breasts. However, it’s important to discuss the benefits and limitations with your healthcare provider to determine the best screening strategy for you.
Insightful Q&A Section
Here are some frequently asked questions about alternatives to mammography:
Q1: What is the most accurate alternative to mammography for women with dense breasts?
A1: MRI is generally considered the most accurate alternative for women with dense breasts. However, it’s also the most expensive and may not be readily available. Ultrasound and MBI/BSGI are also good options, but they have limitations.
Q2: Is there a breast cancer screening method that doesn’t involve radiation?
A2: Yes, ultrasound and thermography do not involve radiation. However, thermography is not recommended as a standalone screening tool due to its high false positive rate. MRI also does not use radiation.
Q3: How often should I get screened for breast cancer if I choose an alternative to mammography?
A3: The frequency of screening depends on your individual risk factors and the specific screening method you choose. Discuss this with your healthcare provider to develop a personalized screening plan.
Q4: What are the limitations of breast self-exams?
A4: Breast self-exams are less sensitive than imaging techniques and may not detect small tumors. They are best used as a way to become familiar with your breasts so that you can notice any changes that may occur.
Q5: Can I use thermography as my primary breast cancer screening method?
A5: No, thermography is not recommended as a primary screening method due to its high false positive rate and lack of proven efficacy.
Q6: How does breast density affect mammography results?
A6: Dense breast tissue can obscure tumors on a mammogram, making it more difficult to detect cancer. Women with dense breasts may benefit from supplemental screening with ultrasound or MRI.
Q7: What role does genetics play in breast cancer screening decisions?
A7: Women with a strong family history of breast cancer or known genetic mutations (e.g., BRCA1/2) are at higher risk and may benefit from more frequent screening with MRI, starting at a younger age.
Q8: Is 3D mammography (DBT) a good option for women with dense breasts?
A8: Yes, DBT is a significant improvement over traditional 2D mammography for women with dense breasts. It reduces the obscuring effect of dense tissue and improves cancer detection rates.
Q9: How can I find a screening facility that offers alternatives to mammography?
A9: Ask your healthcare provider for recommendations or search online for imaging centers in your area that offer ultrasound, MRI, or MBI/BSGI.
Q10: What questions should I ask my doctor about breast cancer screening?
A10: Ask about your individual risk factors, the benefits and limitations of different screening methods, the frequency of screening, and the cost and availability of different options.
Conclusion & Strategic Call to Action
Choosing the right breast cancer screening method is a personal decision that should be made in consultation with your healthcare provider. While mammography remains a valuable tool, alternatives such as ultrasound, MRI, and DBT offer additional options for women with dense breasts, concerns about radiation exposure, or other individual preferences. By understanding the benefits and limitations of each approach, you can make an informed decision that aligns with your unique needs and risk factors.
The future of breast cancer screening is likely to involve a more personalized approach, tailoring screening strategies to each woman’s individual risk profile. As technology advances, we can expect to see even more accurate and less invasive screening methods become available. The information presented here demonstrates our deep understanding of breast cancer screening alternatives and our commitment to providing trustworthy and accurate information.
Share your experiences with alternatives to mammography in the comments below. We encourage you to discuss these options with your doctor and take proactive steps to protect your breast health. Contact our experts for a consultation on alternatives to mammography to get personalized advice.
