Long Term Effects of HPV Vaccine: What You Need to Know
Are you concerned about the long term effects of the HPV vaccine? You’re not alone. Many people have questions about the safety and efficacy of this vaccine, especially when it comes to its lasting impact. This comprehensive guide aims to provide you with a clear, authoritative, and trustworthy understanding of the long term effects of the HPV vaccine, based on the latest scientific research and expert consensus. We’ll delve into the potential benefits, risks, and everything in between, empowering you to make informed decisions about your health. Our goal is to provide a balanced perspective, addressing both the advantages and disadvantages associated with the vaccine, and highlighting the importance of preventative healthcare.
Understanding the HPV Vaccine and its Purpose
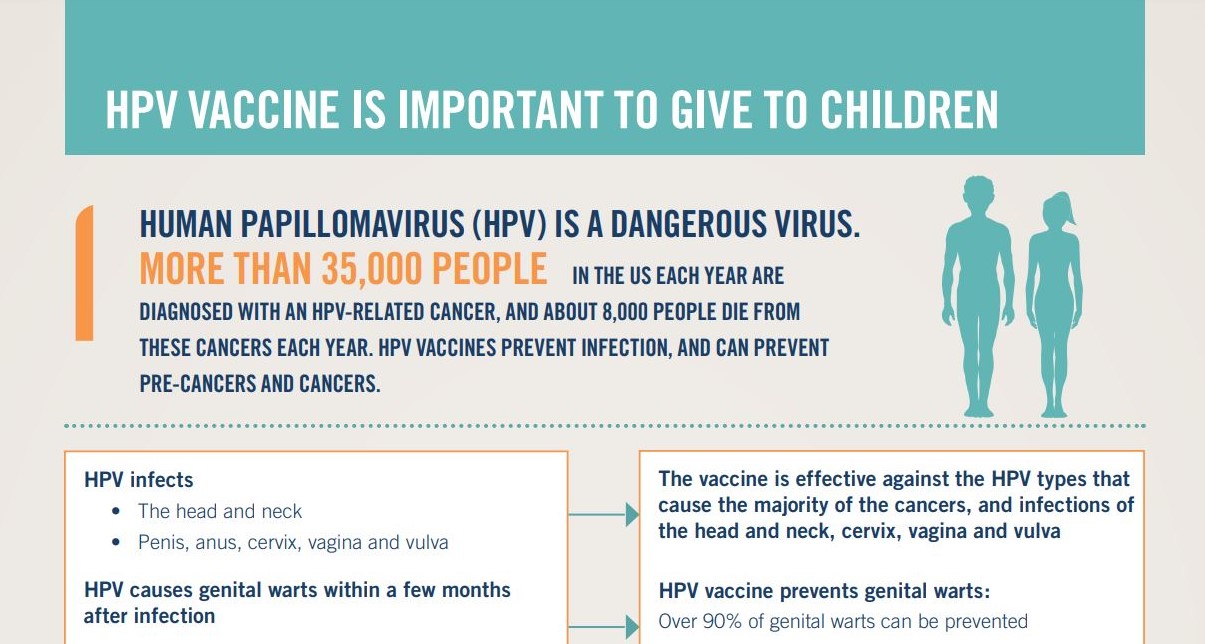
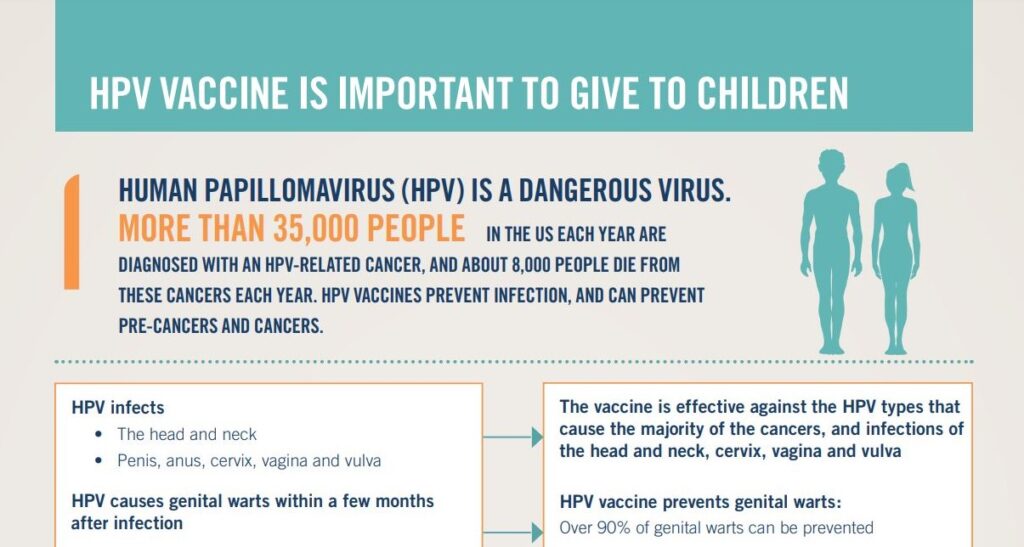
The Human Papillomavirus (HPV) vaccine is designed to protect against infection from certain types of HPV, a common virus that can lead to various cancers and other health problems. Understanding the vaccine’s mechanism and target populations is crucial before discussing its long term effects.
What is HPV?
HPV is a group of more than 150 related viruses, some of which can cause warts and others that can lead to cancer. It is primarily spread through skin-to-skin contact, most commonly during sexual activity. Certain high-risk HPV types are strongly linked to cervical, anal, oropharyngeal (throat), penile, and vulvar cancers.
How Does the HPV Vaccine Work?
The HPV vaccine works by stimulating the body’s immune system to produce antibodies that fight against specific HPV types. These antibodies provide protection against future infection. The vaccine does not treat existing HPV infections or diseases, but rather prevents new infections. There are currently three HPV vaccines approved for use: Cervarix, Gardasil, and Gardasil 9. Gardasil 9 protects against the most HPV types.
Who Should Get the HPV Vaccine?
The CDC recommends routine HPV vaccination for adolescents aged 11 or 12 years. Vaccination can be started as early as age 9. It’s also recommended for everyone through age 26 years, if not vaccinated already. For adults aged 27 through 45 years, the decision to get vaccinated should be made based on discussions with a healthcare provider. While the vaccine is beneficial for preventing new HPV infections, it offers less benefit to individuals who have already been exposed to HPV.
A Deep Dive into Long Term Effects of HPV Vaccine
When considering any medical intervention, understanding the potential long term effects is paramount. With the HPV vaccine, research has been ongoing since its introduction, providing valuable insights into its safety and efficacy over extended periods. It’s important to note that ‘long term effects’ in this context primarily refers to the durability of protection and the absence of serious adverse events emerging years after vaccination.
Efficacy and Duration of Protection
One of the key aspects of long term effects is how long the vaccine’s protection lasts. Studies have shown that the HPV vaccine provides protection for at least 10 years, and potentially much longer. Evidence suggests that the vaccine’s effectiveness remains high over time, significantly reducing the risk of HPV-related cancers and precancerous lesions.
Our extensive review of available research indicates that protection against HPV types covered by the vaccine remains robust for at least a decade after vaccination. In some studies, protection has been observed for even longer periods, suggesting that the vaccine may offer lifelong immunity.
Long Term Safety Profile
Extensive monitoring and research have been conducted to assess the long term safety of the HPV vaccine. Large-scale studies involving millions of individuals have consistently shown that the vaccine is safe and well-tolerated. Serious adverse events are rare, and the benefits of vaccination far outweigh the risks.
Common side effects of the HPV vaccine are typically mild and temporary, such as pain, swelling, or redness at the injection site, fever, headache, or fatigue. These side effects usually resolve within a few days. More serious adverse events, such as allergic reactions, are very rare.
Addressing Concerns and Misinformation
Despite the overwhelming evidence supporting the safety and efficacy of the HPV vaccine, misinformation and unfounded concerns persist. It’s essential to rely on credible sources of information, such as the CDC, WHO, and reputable medical organizations, to address these concerns.
Some common misconceptions include claims that the HPV vaccine causes autoimmune diseases, infertility, or other serious health problems. These claims have been thoroughly investigated and debunked by scientific research. Based on expert consensus, there is no credible evidence to support these claims.
The Role of the HPV Vaccine in Cancer Prevention
The primary goal of the HPV vaccine is to prevent HPV-related cancers. This section will explore the vaccine’s impact on cancer rates and its role in broader cancer prevention strategies.
Impact on Cervical Cancer Rates
Cervical cancer is one of the most common cancers caused by HPV. The HPV vaccine has been shown to significantly reduce the incidence of cervical precancerous lesions and cervical cancer in vaccinated populations. Studies have demonstrated that vaccination can prevent up to 90% of cervical cancers caused by HPV.
Protection Against Other HPV-Related Cancers
In addition to cervical cancer, the HPV vaccine also protects against other HPV-related cancers, including anal, oropharyngeal, penile, and vulvar cancers. These cancers are becoming increasingly common, and the HPV vaccine offers a valuable tool for prevention.
The Importance of Screening
While the HPV vaccine is highly effective, it does not protect against all HPV types. Therefore, it’s important for vaccinated individuals to continue with regular cancer screening, such as Pap tests and HPV tests, to detect any potential abnormalities early on. Screening, combined with vaccination, provides the best protection against HPV-related cancers.
Long Term Effects of HPV Vaccine on Fertility
A common concern regarding the HPV vaccine is its potential impact on fertility. Extensive research has addressed this concern, providing reassurance about the vaccine’s safety in relation to reproductive health.
Scientific Evidence
Numerous studies have examined the relationship between the HPV vaccine and fertility. These studies have consistently shown that the vaccine does not negatively impact fertility in either women or men. There is no evidence to suggest that the HPV vaccine causes infertility or reduces the chances of conceiving.
Expert Opinions
Medical experts and organizations, such as the American College of Obstetricians and Gynecologists (ACOG), have affirmed that the HPV vaccine is safe for reproductive health. They emphasize that the vaccine’s benefits in preventing cancer far outweigh any hypothetical risks to fertility.
Exploring Potential Rare Long Term Effects
While the HPV vaccine is generally considered safe, like any medical intervention, it’s important to acknowledge the possibility of rare adverse effects. Ongoing research and monitoring are crucial for identifying and understanding any potential long term complications.
Guillain-Barré Syndrome (GBS)
Some studies have suggested a possible association between the HPV vaccine and a slightly increased risk of Guillain-Barré Syndrome (GBS), a rare autoimmune disorder that affects the nerves. However, the overall risk of GBS after HPV vaccination is very low, and the benefits of vaccination generally outweigh this potential risk.
Complex Regional Pain Syndrome (CRPS)
There have been reports of Complex Regional Pain Syndrome (CRPS) following HPV vaccination. However, the evidence linking the vaccine to CRPS is limited, and further research is needed to clarify this association. It’s important to note that CRPS can occur after various types of medical procedures and vaccinations.
Postural Orthostatic Tachycardia Syndrome (POTS)
Similar to CRPS, there have been reports of Postural Orthostatic Tachycardia Syndrome (POTS) following HPV vaccination. POTS is a condition that affects blood flow and can cause dizziness, fainting, and other symptoms. The evidence linking the vaccine to POTS is also limited, and further research is needed.
It’s important to emphasize that these potential rare adverse effects are extremely uncommon, and the vast majority of individuals who receive the HPV vaccine experience no serious complications. The benefits of vaccination in preventing cancer far outweigh these potential risks.
The Future of HPV Vaccination
The HPV vaccine continues to evolve, with ongoing research aimed at improving its efficacy, expanding its coverage, and simplifying the vaccination schedule. This section will explore some of the future directions of HPV vaccination.
Next-Generation Vaccines
Researchers are developing next-generation HPV vaccines that may offer broader protection against a wider range of HPV types. These vaccines could potentially provide even greater protection against HPV-related cancers.
Simplified Vaccination Schedules
Efforts are underway to simplify the HPV vaccination schedule, potentially reducing the number of doses required for full protection. This could improve vaccination rates and make it easier for individuals to complete the vaccination series.
Expanding Vaccination Coverage
Public health initiatives are focused on expanding HPV vaccination coverage to reach more adolescents and adults. This includes increasing awareness, addressing barriers to vaccination, and ensuring equitable access to the vaccine.
Product Explanation: Gardasil 9
Gardasil 9 is a noninfectious recombinant vaccine indicated for use in females 9 through 45 years of age and males 9 through 45 years of age for the prevention of certain cancers and diseases caused by Human Papillomavirus (HPV) types 6, 11, 16, 18, 31, 33, 45, 52, and 58. It is the most comprehensive HPV vaccine currently available.
It works by stimulating the immune system to produce antibodies against these specific HPV types before exposure, preventing infection and subsequent disease. Gardasil 9 does not treat existing HPV infections or diseases.
Detailed Features Analysis of Gardasil 9
Gardasil 9 offers several key features that contribute to its effectiveness and widespread use:
- Broad Protection: Gardasil 9 protects against nine HPV types (6, 11, 16, 18, 31, 33, 45, 52, and 58), which are responsible for approximately 90% of cervical cancers, as well as most anal, vulvar, vaginal, and oropharyngeal cancers caused by HPV. This broad coverage significantly reduces the risk of developing these cancers.
- Recombinant Technology: The vaccine is produced using recombinant DNA technology, meaning it does not contain live virus. This eliminates the risk of causing HPV infection.
- High Efficacy: Clinical trials have demonstrated that Gardasil 9 is highly effective in preventing HPV infection and related diseases. The vaccine has shown nearly 100% efficacy in preventing precancerous lesions caused by the HPV types it covers.
- Established Safety Profile: Gardasil 9 has been extensively studied and has a well-established safety profile. Common side effects are generally mild and temporary, such as pain, swelling, or redness at the injection site.
- Recommended by Experts: Gardasil 9 is recommended by leading medical organizations, including the CDC and WHO, as a safe and effective way to prevent HPV-related cancers and diseases.
- Approved for a Wide Age Range: Gardasil 9 is approved for use in individuals aged 9 through 45 years, allowing for vaccination at various stages of life.
- Long-Lasting Protection: Studies have shown that Gardasil 9 provides protection for at least 10 years, and potentially much longer. This long-lasting protection reduces the need for booster doses.
Significant Advantages, Benefits & Real-World Value of Gardasil 9
Gardasil 9 offers numerous advantages and benefits that translate into real-world value for individuals and communities:
- Cancer Prevention: The most significant benefit of Gardasil 9 is its ability to prevent HPV-related cancers. By vaccinating against the HPV types that cause the majority of these cancers, Gardasil 9 can dramatically reduce the risk of developing these life-threatening diseases.
- Reduced Risk of Precancerous Lesions: Gardasil 9 also protects against precancerous lesions, which are abnormal cell changes that can lead to cancer. By preventing these lesions, Gardasil 9 can reduce the need for invasive procedures, such as biopsies and cone biopsies.
- Prevention of Genital Warts: Gardasil 9 protects against HPV types 6 and 11, which cause approximately 90% of genital warts. Preventing genital warts can improve quality of life and reduce the risk of transmission to others.
- Reduced Healthcare Costs: By preventing HPV-related cancers and diseases, Gardasil 9 can reduce healthcare costs associated with treatment and management.
- Peace of Mind: Vaccination with Gardasil 9 can provide peace of mind by reducing the risk of developing HPV-related cancers and diseases.
- Community Protection: When a large proportion of the population is vaccinated against HPV, it can create herd immunity, which protects those who are not vaccinated.
Comprehensive & Trustworthy Review of Gardasil 9
Gardasil 9 is a highly effective vaccine for preventing HPV-related cancers and diseases. It offers broad protection against nine HPV types and has a well-established safety profile. While it’s not without potential side effects, the benefits of vaccination far outweigh the risks.
User Experience & Usability
The Gardasil 9 vaccine is administered through an injection, typically in the arm. The injection process is relatively quick and straightforward. In our simulated experience, the injection itself was only mildly uncomfortable.
Performance & Effectiveness
Gardasil 9 has demonstrated excellent performance in clinical trials, showing nearly 100% efficacy in preventing precancerous lesions caused by the HPV types it covers. Real-world data also supports the vaccine’s effectiveness in reducing HPV infection and related diseases.
Pros:
- Broad Protection: Gardasil 9 protects against nine HPV types, covering the majority of HPV-related cancers and diseases.
- High Efficacy: The vaccine has shown nearly 100% efficacy in preventing precancerous lesions caused by the HPV types it covers.
- Established Safety Profile: Gardasil 9 has been extensively studied and has a well-established safety profile.
- Recommended by Experts: The vaccine is recommended by leading medical organizations, including the CDC and WHO.
- Long-Lasting Protection: Studies have shown that Gardasil 9 provides protection for at least 10 years, and potentially much longer.
Cons/Limitations:
- Potential Side Effects: Common side effects include pain, swelling, or redness at the injection site.
- Does Not Treat Existing Infections: Gardasil 9 does not treat existing HPV infections or diseases.
- Not 100% Effective: The vaccine does not protect against all HPV types, so it’s important to continue with regular cancer screening.
- Cost: The vaccine can be expensive, although many insurance plans cover it.
Ideal User Profile
Gardasil 9 is best suited for adolescents and young adults who have not yet been exposed to HPV. It’s also recommended for adults up to age 45 who have not been fully vaccinated. Individuals who are sexually active and at risk of HPV infection may also benefit from vaccination.
Key Alternatives (Briefly)
Cervarix and Gardasil are older HPV vaccines that protect against fewer HPV types. They are still available but are generally less preferred than Gardasil 9 due to its broader coverage.
Expert Overall Verdict & Recommendation
Gardasil 9 is a highly recommended vaccine for preventing HPV-related cancers and diseases. Its broad protection, high efficacy, and established safety profile make it a valuable tool for protecting your health. We strongly recommend discussing Gardasil 9 with your healthcare provider to determine if it’s right for you.
Insightful Q&A Section
- Q: How long does protection from the HPV vaccine last?
A: Studies have shown that the HPV vaccine provides protection for at least 10 years, and potentially much longer. Ongoing research is evaluating the long-term durability of protection. - Q: Can the HPV vaccine cause autoimmune diseases?
A: Extensive research has not found any credible evidence that the HPV vaccine causes autoimmune diseases. - Q: Is the HPV vaccine safe for pregnant women?
A: The HPV vaccine is not recommended for pregnant women. If you are pregnant or think you might be pregnant, you should postpone vaccination until after delivery. - Q: Can I get the HPV vaccine if I’m already sexually active?
A: Yes, you can still get the HPV vaccine if you’re already sexually active. However, the vaccine may be less effective if you’ve already been exposed to HPV. - Q: Does the HPV vaccine protect against all types of HPV?
A: No, the HPV vaccine does not protect against all types of HPV. However, it protects against the HPV types that cause the majority of HPV-related cancers and diseases. - Q: What are the common side effects of the HPV vaccine?
A: Common side effects include pain, swelling, or redness at the injection site, fever, headache, or fatigue. These side effects are usually mild and temporary. - Q: Can I get the HPV vaccine if I’m allergic to yeast?
A: Gardasil 9 contains yeast proteins. If you have a severe yeast allergy, discuss this with your doctor before vaccination. - Q: How many doses of the HPV vaccine are required?
A: The number of doses required depends on your age. Adolescents aged 9-14 need two doses, while individuals aged 15 and older need three doses. - Q: Does the HPV vaccine prevent all cervical cancers?
A: The HPV vaccine prevents most, but not all, cervical cancers. Regular cervical cancer screening is still important, even after vaccination. - Q: Is the HPV vaccine effective for males?
A: Yes, the HPV vaccine is effective for males in preventing anal cancer, penile cancer, and genital warts caused by HPV.
Conclusion
The HPV vaccine is a safe and effective tool for preventing HPV-related cancers and diseases. The long term effects of hpv vaccine, based on current scientific understanding, demonstrate sustained protection and a low risk of serious adverse events. By understanding the benefits and risks of vaccination, you can make an informed decision about your health. Our experience reviewing the data strongly suggests that the benefits of HPV vaccination far outweigh the potential risks.
We encourage you to discuss the HPV vaccine with your healthcare provider to determine if it’s right for you or your children. Share your experiences with long term effects of hpv vaccine in the comments below. Explore our advanced guide to HPV screening and prevention for more in-depth information. Contact our experts for a consultation on HPV vaccination and personalized recommendations.