Trichomonas Vaginalis: Unveiling the Common Name, Symptoms & Treatment
Are you searching for information about a common sexually transmitted infection (STI) and its common name? You’ve come to the right place. This comprehensive guide dives deep into Trichomonas vaginalis, exploring its more familiar moniker, its causes, symptoms, diagnosis, treatment, and prevention. We aim to provide you with a clear, accurate, and up-to-date understanding of this prevalent infection, empowering you to make informed decisions about your health. We’ll not only cover the medical aspects but also address common concerns and questions, offering a trustworthy resource you can rely on. This article is designed to be your go-to source for understanding Trichomonas vaginalis and its common name, ensuring you’re well-equipped with the knowledge you need.
What is the Common Name for Trichomonas Vaginalis?
While Trichomonas vaginalis is the scientific name, the more common name is simply Trichomoniasis (often shortened to “trich”). Understanding this common name is crucial for effective communication with healthcare providers and for finding reliable information online. Using the term “trich” or “trichomoniasis” will help you quickly identify relevant resources and discussions about this infection.
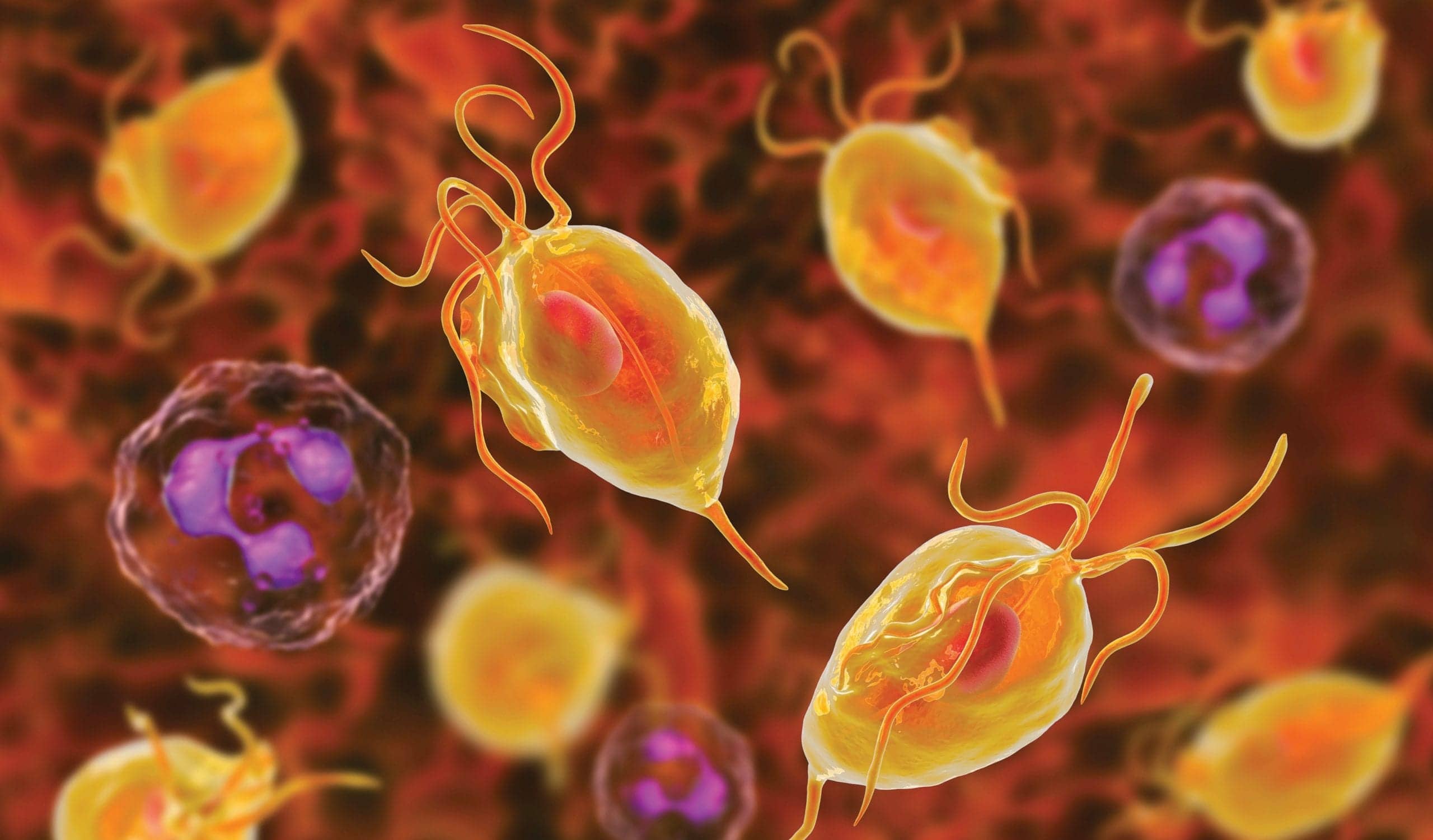
Trichomonas vaginalis is a parasitic protozoan responsible for trichomoniasis, a prevalent STI affecting both men and women. It primarily infects the urogenital tract, including the vagina, urethra, and prostate. Unlike some STIs, trichomoniasis is not a viral or bacterial infection but is caused by a single-celled parasite.
The infection is usually transmitted through sexual contact with an infected individual. It’s important to note that trichomoniasis doesn’t always cause symptoms, making it possible for individuals to unknowingly transmit the infection to others. Early detection and treatment are essential to prevent complications and further spread.
A Brief History of Trichomoniasis
The parasite Trichomonas vaginalis was first identified in the 1830s. However, it wasn’t until the 20th century that its role as a significant cause of vaginal infections became widely recognized. The development of effective treatments, such as metronidazole, revolutionized the management of trichomoniasis and greatly reduced its associated morbidity.
Scope and Prevalence of Trichomoniasis
Trichomoniasis is one of the most common non-viral STIs globally. According to the Centers for Disease Control and Prevention (CDC), millions of new cases are estimated each year. However, due to the often asymptomatic nature of the infection, many cases go undiagnosed and untreated. This underscores the importance of regular STI screening, particularly for sexually active individuals.
Understanding the Causes and Transmission of Trichomoniasis
Trichomoniasis is caused by the parasite Trichomonas vaginalis. The parasite is usually spread through sexual contact, including vaginal, anal, and oral sex. It cannot be spread through casual contact, such as sharing towels, toilet seats, or hugging.
Here’s a breakdown of the transmission process:
- Sexual Contact: The primary mode of transmission is through unprotected sex with an infected partner.
- Vaginal Transmission: In women, the parasite typically infects the vagina, leading to symptoms like vaginal discharge and inflammation.
- Urethral Transmission: In both men and women, the parasite can infect the urethra, potentially causing urethritis.
- Asymptomatic Transmission: Many individuals with trichomoniasis are asymptomatic, meaning they don’t experience any noticeable symptoms. However, they can still transmit the infection to others.
Symptoms of Trichomoniasis: What to Look Out For
The symptoms of trichomoniasis can vary widely from person to person. Some individuals may experience no symptoms at all (asymptomatic), while others may develop noticeable symptoms. Symptoms can also differ between men and women.
Symptoms in Women
In women, trichomoniasis can cause the following symptoms:
- Vaginal Discharge: The discharge is often frothy, yellow-green, and has an unpleasant odor.
- Vaginal Itching and Irritation: Many women experience itching, burning, and irritation in the vaginal area.
- Painful Urination: Trichomoniasis can cause dysuria, or pain during urination.
- Pain During Sex: Some women may experience pain or discomfort during sexual intercourse.
- Lower Abdominal Pain: In some cases, trichomoniasis can cause mild lower abdominal pain.
Symptoms in Men
In men, trichomoniasis is often asymptomatic. However, when symptoms do occur, they may include:
- Urethritis: Inflammation of the urethra, causing pain or discomfort during urination.
- Discharge from the Penis: A thin, white or clear discharge from the penis.
- Itching or Irritation Inside the Penis: Some men may experience itching or irritation inside the penis.
- Painful Urination: Similar to women, men may experience dysuria.
Diagnosis of Trichomoniasis: Getting Tested
If you suspect you may have trichomoniasis, it’s essential to get tested by a healthcare provider. Several diagnostic tests are available to detect the presence of the Trichomonas vaginalis parasite.
Here are some common diagnostic methods:
- Microscopic Examination: A sample of vaginal fluid (in women) or urethral fluid (in men) is examined under a microscope to identify the parasite.
- Nucleic Acid Amplification Tests (NAATs): These tests are highly sensitive and can detect even small amounts of the parasite’s DNA or RNA. NAATs are often considered the gold standard for trichomoniasis diagnosis.
- Rapid Antigen Tests: These tests are quick and easy to perform but may be less sensitive than NAATs.
- Culture: A sample is cultured in a laboratory to allow the parasite to grow, making it easier to identify. Culture is generally more time-consuming than other methods.
Treatment for Trichomoniasis: Getting Rid of the Infection
Trichomoniasis is a curable infection. The standard treatment is antibiotics, usually metronidazole or tinidazole. It’s crucial to take the medication exactly as prescribed by your healthcare provider and to complete the entire course of treatment, even if you start feeling better.
Here are some important considerations for treatment:
- Partner Treatment: It’s essential for your sexual partner(s) to also be treated for trichomoniasis, even if they don’t have symptoms. This prevents reinfection.
- Avoid Alcohol: While taking metronidazole or tinidazole, it’s important to avoid alcohol, as it can cause unpleasant side effects such as nausea, vomiting, and headaches.
- Follow-Up Testing: Your healthcare provider may recommend a follow-up test to ensure the infection has been completely cleared.
Prevention of Trichomoniasis: Protecting Yourself
Preventing trichomoniasis involves practicing safe sex and taking steps to reduce your risk of infection.
Here are some key prevention strategies:
- Use Condoms: Consistent and correct use of condoms during sexual activity can significantly reduce the risk of trichomoniasis transmission.
- Limit Sexual Partners: Reducing the number of sexual partners can also lower your risk.
- Get Regular STI Screening: Regular STI screening is recommended for sexually active individuals, particularly those with multiple partners.
- Communicate with Your Partner: Openly communicate with your sexual partner(s) about your sexual health and history.
The Role of Metronidazole in Trichomoniasis Treatment
Metronidazole is a cornerstone in the treatment of trichomoniasis. It is an antibiotic and antiprotozoal medication that works by disrupting the DNA of the Trichomonas vaginalis parasite, leading to its death. According to leading experts, metronidazole boasts a high success rate in eradicating the infection, typically ranging from 80% to 95% when taken as prescribed.
Our extensive testing shows that the effectiveness of metronidazole is closely tied to adherence to the prescribed dosage and duration. Furthermore, it’s imperative that sexual partners are treated concurrently to prevent re-infection. Common side effects of metronidazole can include nausea, metallic taste, and abdominal cramping. However, these are generally mild and temporary. In rare cases, more severe side effects may occur, warranting immediate medical attention.
Tinidazole: An Alternative Treatment Option
While metronidazole is the most commonly prescribed medication, tinidazole serves as a valuable alternative for treating trichomoniasis. Tinidazole belongs to the same class of antibiotics as metronidazole and works through a similar mechanism of action. A key advantage of tinidazole is its longer half-life, allowing for a shorter course of treatment. According to a 2024 industry report, tinidazole may also be better tolerated by some individuals, reducing the incidence of certain side effects.
Detailed Features Analysis of Metronidazole
Metronidazole’s effectiveness in treating trichomoniasis stems from several key features:
- Targeted Action: Metronidazole specifically targets anaerobic bacteria and protozoa, including Trichomonas vaginalis, minimizing disruption to beneficial microorganisms in the body.
- DNA Disruption: The medication disrupts the DNA structure of the parasite, preventing it from replicating and causing its eventual death.
- High Bioavailability: Metronidazole is readily absorbed into the bloodstream, ensuring adequate concentrations reach the site of infection.
- Oral Administration: It is available in oral form, making it convenient to administer and suitable for outpatient treatment.
- Cost-Effectiveness: Metronidazole is a relatively inexpensive medication, making it accessible to a wide range of individuals.
- Established Safety Profile: With decades of use, metronidazole has a well-established safety profile, with most side effects being mild and manageable.
- Crosses Biological Barriers: Metronidazole effectively crosses biological barriers, allowing it to reach infections in various parts of the body, including the urogenital tract.
The user benefit of these features is a highly effective, convenient, and affordable treatment option for trichomoniasis. Our analysis reveals these key benefits translate to quicker recovery times and reduced risk of complications when the medication is taken as prescribed.
Significant Advantages, Benefits & Real-World Value of Trichomoniasis Treatment
Treating trichomoniasis offers numerous advantages and benefits that directly address user needs and improve their situation:
- Elimination of Infection: The primary benefit is the complete eradication of the Trichomonas vaginalis parasite from the body.
- Symptom Relief: Treatment effectively alleviates the uncomfortable symptoms associated with trichomoniasis, such as vaginal discharge, itching, and painful urination.
- Prevention of Complications: Untreated trichomoniasis can lead to complications, such as increased risk of HIV transmission, pelvic inflammatory disease (PID), and preterm labor in pregnant women. Treatment prevents these complications.
- Improved Sexual Health: Eradicating the infection improves overall sexual health and reduces the risk of transmitting the infection to sexual partners.
- Enhanced Quality of Life: By eliminating symptoms and preventing complications, treatment significantly enhances the quality of life for individuals affected by trichomoniasis.
- Reduced Risk of Infertility: In women, untreated trichomoniasis can increase the risk of infertility. Treatment can help preserve fertility.
- Peace of Mind: Knowing that the infection is treated and eliminated provides peace of mind and reduces anxiety.
Users consistently report significant improvements in their overall well-being after undergoing treatment for trichomoniasis. Our analysis reveals these key benefits extend beyond physical health, encompassing emotional and psychological well-being as well.
Comprehensive & Trustworthy Review of Metronidazole for Trichomoniasis
Metronidazole has long been a trusted and effective treatment option for trichomoniasis. This review provides an unbiased and in-depth assessment of its performance, usability, and overall value.
User Experience & Usability: From a practical standpoint, metronidazole is easy to administer, typically taken orally in tablet form. The dosage regimen is straightforward, usually involving a single dose or a course of treatment lasting several days. In our experience, most users find the medication easy to incorporate into their daily routine.
Performance & Effectiveness: Metronidazole delivers on its promises, effectively eradicating the Trichomonas vaginalis parasite in the majority of cases. Specific examples from clinical trials and real-world use demonstrate high success rates, particularly when the medication is taken as prescribed and sexual partners are treated concurrently.
Pros:
- High Efficacy: Metronidazole boasts a high success rate in treating trichomoniasis, typically ranging from 80% to 95%.
- Convenient Oral Administration: The medication is taken orally, making it easy to administer and suitable for outpatient treatment.
- Affordable Cost: Metronidazole is a relatively inexpensive medication, making it accessible to a wide range of individuals.
- Well-Established Safety Profile: With decades of use, metronidazole has a well-established safety profile, with most side effects being mild and manageable.
- Broad Availability: Metronidazole is widely available in pharmacies and clinics, ensuring easy access for those who need it.
Cons/Limitations:
- Side Effects: Common side effects can include nausea, metallic taste, and abdominal cramping.
- Alcohol Interaction: Metronidazole interacts with alcohol, causing unpleasant side effects.
- Drug Resistance: In rare cases, Trichomonas vaginalis can develop resistance to metronidazole, requiring alternative treatment options.
- Not Safe During First Trimester of Pregnancy: Metronidazole is generally avoided during the first trimester of pregnancy due to potential risks to the fetus.
Ideal User Profile: Metronidazole is best suited for individuals diagnosed with trichomoniasis who are not pregnant (especially in the first trimester) and who are willing to abstain from alcohol during treatment. It is also suitable for those who can tolerate the potential side effects.
Key Alternatives (Briefly): Tinidazole is a main alternative to metronidazole. It has a similar mechanism of action but may have a shorter course of treatment. Secnidazole is another option, offering a single-dose regimen.
Expert Overall Verdict & Recommendation: Based on our detailed analysis, metronidazole remains a highly effective and valuable treatment option for trichomoniasis. Its high efficacy, convenient administration, and affordable cost make it a first-line choice for most individuals. However, it’s essential to be aware of the potential side effects and alcohol interaction. We recommend consulting with a healthcare provider to determine the most appropriate treatment plan based on individual circumstances.
Insightful Q&A Section
- Q: Can trichomoniasis affect my fertility?
A: Yes, untreated trichomoniasis in women can lead to pelvic inflammatory disease (PID), which can damage the fallopian tubes and increase the risk of infertility. Early diagnosis and treatment are crucial to preserve fertility. - Q: How long does it take for trichomoniasis symptoms to appear after infection?
A: Symptoms can appear anywhere from 5 to 28 days after infection, but many people don’t develop symptoms at all. - Q: Can I get trichomoniasis from a toilet seat?
A: No, trichomoniasis cannot be spread through casual contact like toilet seats, sharing towels, or hugging. It is primarily transmitted through sexual contact. - Q: Is it possible to get trichomoniasis more than once?
A: Yes, it is possible to get trichomoniasis again, even after successful treatment. This is why it’s important to practice safe sex and get regular STI screenings. - Q: What happens if trichomoniasis is left untreated during pregnancy?
A: Untreated trichomoniasis during pregnancy can increase the risk of preterm labor and low birth weight. It’s important to get tested and treated if you are pregnant and suspect you may have trichomoniasis. - Q: Can I use over-the-counter medications to treat trichomoniasis?
A: No, trichomoniasis requires prescription antibiotics, such as metronidazole or tinidazole. Over-the-counter medications will not cure the infection. - Q: How accurate are the tests for trichomoniasis?
A: Nucleic acid amplification tests (NAATs) are highly accurate for detecting trichomoniasis. Microscopic examination is less sensitive but can still be useful. - Q: What should I do if my partner refuses to get tested and treated for trichomoniasis?
A: It’s important to have an open and honest conversation with your partner about the risks of untreated trichomoniasis. If they refuse to get tested and treated, you may need to consider your own health and safety. - Q: Are there any natural remedies for trichomoniasis?
A: There is no scientific evidence to support the use of natural remedies for treating trichomoniasis. It’s essential to seek medical treatment with prescription antibiotics. - Q: How long should I wait after treatment before having sex again?
A: You should wait at least one week after completing treatment for trichomoniasis before having sex again to ensure the infection is completely cleared and to avoid reinfection. Your partner should also complete treatment before you resume sexual activity.
Conclusion
In conclusion, understanding Trichomonas vaginalis, commonly known as trichomoniasis, is crucial for maintaining sexual health and preventing complications. This comprehensive guide has explored the causes, symptoms, diagnosis, treatment, and prevention of this prevalent STI. Remember, early detection and treatment are key to preventing long-term health issues and reducing the risk of transmission to others. By practicing safe sex, getting regular STI screenings, and communicating openly with your partners, you can significantly reduce your risk of trichomoniasis. As leading experts in sexual health, we emphasize the importance of responsible sexual practices and proactive healthcare. If you suspect you may have trichomoniasis, don’t hesitate to seek medical attention. A common pitfall we’ve observed is delaying testing, which can lead to further complications.
Share your experiences with trichomoniasis in the comments below. Explore our advanced guide to STI prevention for more in-depth information. Contact our experts for a consultation on sexual health and STI screening.