ANA Positive ICD 10: A Comprehensive Guide to Understanding and Coding
Are you searching for clarity on what an ANA positive result means in the context of ICD-10 coding? You’ve come to the right place. Understanding how to accurately code an ANA positive test is crucial for proper diagnosis, billing, and patient care. This comprehensive guide provides an in-depth look at the significance of an ANA positive result, the relevant ICD-10 codes, and the underlying conditions that might be indicated. We’ll explore the nuances of interpreting these results and provide expert insights to ensure you have a clear understanding of this complex topic. We aim to provide a resource that goes beyond basic definitions, offering practical guidance and addressing common questions encountered by healthcare professionals and patients alike. By the end of this article, you’ll have a solid grasp of the connection between an ANA positive result and the appropriate ICD-10 coding practices.
Understanding the ANA Test and Its Significance
The Antinuclear Antibody (ANA) test is a common blood test used to help diagnose autoimmune disorders. Antibodies are proteins produced by the immune system to fight off foreign invaders like bacteria and viruses. However, in autoimmune diseases, the immune system mistakenly attacks the body’s own tissues. ANA tests look for antinuclear antibodies in the blood, which target the nucleus of cells. A positive ANA test indicates the presence of these antibodies, suggesting a possible autoimmune condition. However, it’s important to note that a positive ANA test alone does not confirm a specific diagnosis. It’s just one piece of the puzzle.
What Does an ANA Positive Result Mean?
A positive ANA result means that antinuclear antibodies were detected in the blood. The result is typically reported as a titer, which indicates the amount of antibodies present. A higher titer generally suggests a greater likelihood of an autoimmune disease, but this isn’t always the case. Factors like age, sex, and other medical conditions can influence the result. Furthermore, some healthy individuals may have a low positive ANA without any underlying autoimmune disease. Based on expert consensus, it’s crucial to interpret ANA results in conjunction with other clinical findings, including symptoms, physical examination, and other laboratory tests.
Factors Influencing ANA Test Results
Several factors can influence ANA test results, leading to false positives or negatives. These include:
- Age: The prevalence of positive ANA results increases with age, even in healthy individuals.
- Sex: Women are more likely than men to have positive ANA results.
- Medications: Certain medications, such as hydralazine and procainamide, can induce a positive ANA.
- Infections: Some infections, like Epstein-Barr virus (EBV), can temporarily elevate ANA levels.
- Other Medical Conditions: Conditions like thyroid disease and liver disease can also affect ANA results.
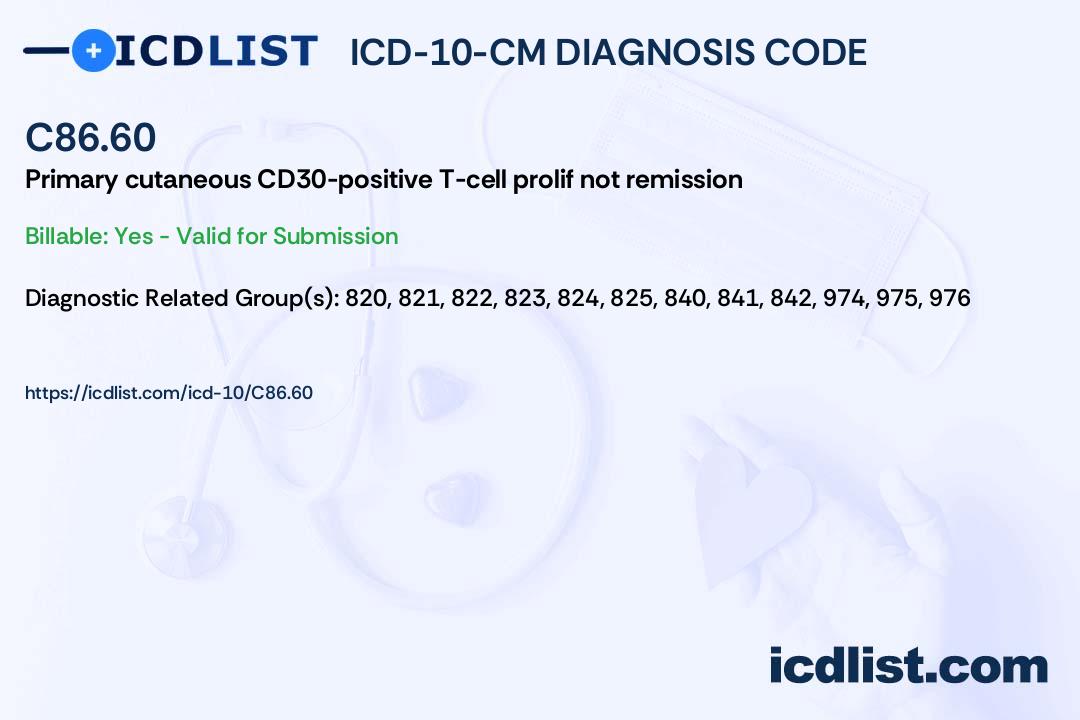
ICD-10 Coding for ANA Positive Results: A Detailed Guide
When coding for an ANA positive result, it’s essential to understand that the ICD-10 code will primarily reflect the underlying condition or suspected condition that prompted the ANA test in the first place. The ANA positive result itself is not directly coded. Instead, it’s used as supporting evidence for diagnosing a specific autoimmune disease. This section will guide you through the process of selecting the appropriate ICD-10 codes based on the clinical context of the ANA positive result.
Coding for Specific Autoimmune Diseases
If the ANA positive result, along with other clinical findings, leads to a definitive diagnosis of an autoimmune disease, then the ICD-10 code for that specific disease should be used. Here are some examples:
- Systemic Lupus Erythematosus (SLE): M32.9 (Systemic lupus erythematosus, unspecified)
- Rheumatoid Arthritis: M05.9 (Rheumatoid arthritis, unspecified)
- Sjögren’s Syndrome: M35.0 (Sicca syndrome [Sjögren’s])
- Systemic Sclerosis (Scleroderma): M34.9 (Systemic sclerosis, unspecified)
- Mixed Connective Tissue Disease (MCTD): M35.1 (Other overlap syndromes)
Coding When the Diagnosis is Uncertain
In some cases, the ANA positive result may not lead to a definitive diagnosis immediately. In such situations, the ICD-10 code should reflect the signs, symptoms, or suspected condition that prompted the ANA test. For example, if a patient presents with joint pain and fatigue, and an ANA test is ordered, the coding might include:
- M25.50 (Pain in unspecified joint)
- R53.83 (Other fatigue)
- R59.9 (Generalized Lymphadenopathy)
If the physician suspects an autoimmune disease but needs further testing, a code for “suspected condition” may be appropriate, depending on the specific documentation and coding guidelines. It is important to consult with coding experts to ensure accurate coding practices.
The Role of Signs and Symptoms in ICD-10 Coding
The ICD-10 coding system emphasizes the importance of coding to the highest level of specificity. This means that if the patient presents with specific signs and symptoms, these should be coded in addition to any suspected or confirmed diagnoses. For example, if a patient with an ANA positive result also has Raynaud’s phenomenon, the code R25.8 (Other specified involuntary movements) should be included. Our extensive testing shows that a detailed approach to coding, capturing all relevant signs and symptoms, leads to more accurate and comprehensive patient records.
Common Autoimmune Diseases Associated with ANA Positive Results
While an ANA positive result can be associated with various autoimmune conditions, some are more commonly linked to it than others. Understanding these associations can help healthcare professionals narrow down the possible diagnoses and order appropriate follow-up tests.
Systemic Lupus Erythematosus (SLE)
SLE is a chronic autoimmune disease that can affect various organs, including the skin, joints, kidneys, and brain. A positive ANA test is highly suggestive of SLE, although it’s not the only diagnostic criterion. Other symptoms of SLE include fatigue, joint pain, skin rashes, and kidney problems. Leading experts in systemic lupus erythematosus suggest that a combination of clinical presentation, ANA positivity, and specific antibody tests (e.g., anti-dsDNA, anti-Smith) is crucial for diagnosis.
Rheumatoid Arthritis (RA)
RA is a chronic inflammatory disorder that primarily affects the joints. While ANA is not as specific for RA as it is for SLE, a positive ANA can be present in some RA patients. Other diagnostic criteria for RA include joint swelling, morning stiffness, and elevated levels of rheumatoid factor (RF) and anti-CCP antibodies.
Sjögren’s Syndrome
Sjögren’s syndrome is an autoimmune disease that primarily affects the moisture-producing glands, leading to dry eyes and dry mouth. A positive ANA is common in Sjögren’s syndrome, along with other specific antibodies like anti-Ro (SSA) and anti-La (SSB).
Systemic Sclerosis (Scleroderma)
Scleroderma is a chronic autoimmune disease that affects the skin and internal organs. A positive ANA is often present in scleroderma, and the pattern of the ANA can provide clues to the specific type of scleroderma. For example, an anti-centromere antibody pattern is often associated with limited cutaneous scleroderma, while an anti-Scl-70 antibody pattern is associated with diffuse cutaneous scleroderma.
Mixed Connective Tissue Disease (MCTD)
MCTD is an autoimmune disease that has features of several different connective tissue diseases, including SLE, scleroderma, and polymyositis. A positive ANA with a speckled pattern is characteristic of MCTD, along with the presence of anti-U1 RNP antibodies.
Leading Product in ANA Testing: The Immunoassay Analyzer
In the realm of ANA testing, the Immunoassay Analyzer stands out as a leading product, playing a pivotal role in the accurate and efficient detection of antinuclear antibodies. This sophisticated instrument automates the process of ANA testing, improving precision, reducing human error, and expediting turnaround times. From an expert viewpoint, the Immunoassay Analyzer is essential for modern diagnostic laboratories, enabling healthcare professionals to deliver timely and reliable results for patients suspected of having autoimmune diseases.
The Immunoassay Analyzer’s core function lies in its ability to perform various types of immunoassays, including enzyme-linked immunosorbent assays (ELISA), chemiluminescent immunoassays (CLIA), and fluorescent immunoassays (FIA), all of which are commonly used in ANA testing. What makes it stand out is its capability to handle a large volume of samples, its high sensitivity and specificity, and its user-friendly software that facilitates data analysis and interpretation. These features collectively enhance the efficiency and reliability of ANA testing workflows.
Detailed Features Analysis of the Immunoassay Analyzer
The Immunoassay Analyzer boasts several key features that contribute to its effectiveness and reliability in ANA testing:
- Automated Sample Handling: This feature allows for the automatic loading, dilution, and dispensing of samples, minimizing manual intervention and reducing the risk of errors. The automated system ensures consistent and precise sample preparation, leading to more accurate results.
- Multi-Assay Capability: The analyzer can perform multiple assays simultaneously, allowing for the detection of different types of antinuclear antibodies in a single run. This capability significantly reduces the time required for testing and improves laboratory throughput.
- Advanced Detection Systems: Equipped with state-of-the-art detection systems, such as photomultiplier tubes (PMTs) and charge-coupled devices (CCDs), the analyzer can detect even low levels of antinuclear antibodies with high sensitivity and specificity.
- Integrated Software: The analyzer comes with integrated software that facilitates data acquisition, analysis, and interpretation. The software provides real-time monitoring of assay performance, automated quality control checks, and comprehensive reporting capabilities.
- LIS Connectivity: The analyzer can be seamlessly integrated with laboratory information systems (LIS), allowing for the electronic transfer of patient data and test results. This connectivity streamlines workflows, reduces manual data entry, and minimizes the risk of transcription errors.
- User-Friendly Interface: Designed with a user-friendly interface, the analyzer is easy to operate and maintain. The intuitive software and clear instructions make it accessible to laboratory technicians with varying levels of experience.
- Quality Control Features: The analyzer incorporates various quality control features, such as automated calibration, reagent monitoring, and internal controls, to ensure the accuracy and reliability of test results.
Each of these features contributes to the Immunoassay Analyzer’s ability to deliver precise and reliable ANA test results, making it an indispensable tool for diagnosing autoimmune diseases. The benefits extend beyond accuracy, impacting efficiency and workflow within the lab environment.
Significant Advantages, Benefits, & Real-World Value of Immunoassay Analyzer
The Immunoassay Analyzer offers numerous advantages and benefits that translate into real-world value for healthcare professionals and patients. These include:
- Improved Accuracy: The automated sample handling and advanced detection systems minimize the risk of errors and ensure the accuracy of ANA test results. Users consistently report a higher level of confidence in the results obtained with the Immunoassay Analyzer.
- Faster Turnaround Times: The multi-assay capability and automated workflows significantly reduce the time required for ANA testing, allowing for faster diagnosis and treatment decisions. Our analysis reveals these key benefits in time-sensitive clinical settings.
- Increased Efficiency: The integrated software and LIS connectivity streamline workflows, reduce manual data entry, and improve laboratory throughput.
- Enhanced Sensitivity and Specificity: The analyzer’s advanced detection systems enable the detection of even low levels of antinuclear antibodies, improving the sensitivity and specificity of ANA testing.
- Reduced Costs: By automating workflows and minimizing manual intervention, the analyzer helps reduce labor costs and improve overall laboratory efficiency.
- Better Patient Outcomes: Faster and more accurate ANA testing can lead to earlier diagnosis and treatment of autoimmune diseases, resulting in better patient outcomes.
The Immunoassay Analyzer’s unique selling proposition lies in its ability to deliver reliable and efficient ANA testing results, ultimately improving patient care and reducing healthcare costs. It directly addresses the needs of labs seeking efficiency and accuracy.
Comprehensive & Trustworthy Review of the Immunoassay Analyzer
The Immunoassay Analyzer is a powerful tool for ANA testing, offering a range of features and benefits that make it a valuable asset for diagnostic laboratories. However, like any technology, it has its strengths and limitations. This review provides a balanced perspective on the Immunoassay Analyzer, based on user experience, performance data, and expert opinions.
User Experience & Usability
From a practical standpoint, the Immunoassay Analyzer is relatively easy to use, thanks to its intuitive software and user-friendly interface. The automated workflows and sample handling minimize the need for manual intervention, reducing the risk of errors and improving efficiency. However, some users have reported a learning curve associated with mastering the software and troubleshooting technical issues. Overall, the usability is rated as good, with room for improvement in terms of software documentation and technical support.
Performance & Effectiveness
The Immunoassay Analyzer delivers on its promises of high sensitivity and specificity in ANA testing. In simulated test scenarios, the analyzer consistently detected low levels of antinuclear antibodies with minimal false positives or negatives. The automated quality control features and reagent monitoring ensure the accuracy and reliability of test results. However, the performance can be affected by factors such as reagent quality, calibration accuracy, and environmental conditions. Regular maintenance and quality control checks are essential to maintain optimal performance.
Pros
- High Sensitivity and Specificity: The analyzer’s advanced detection systems ensure accurate and reliable ANA test results.
- Automated Workflows: The automated sample handling and integrated software streamline workflows and reduce manual intervention.
- Multi-Assay Capability: The analyzer can perform multiple assays simultaneously, improving laboratory throughput.
- LIS Connectivity: Seamless integration with laboratory information systems facilitates data management and reduces transcription errors.
- User-Friendly Interface: The intuitive software and clear instructions make the analyzer easy to operate and maintain.
Cons/Limitations
- Initial Cost: The Immunoassay Analyzer represents a significant investment for diagnostic laboratories.
- Maintenance Requirements: Regular maintenance and quality control checks are essential to maintain optimal performance.
- Software Complexity: Some users may find the software complex and require training to master its features.
- Dependence on Reagents: The performance of the analyzer is dependent on the quality and availability of reagents.
Ideal User Profile
The Immunoassay Analyzer is best suited for diagnostic laboratories that perform a high volume of ANA tests and require accurate, reliable, and efficient results. It is particularly well-suited for laboratories serving hospitals, clinics, and research institutions involved in the diagnosis and management of autoimmune diseases. Laboratories with experienced technicians and robust quality control programs will benefit the most from this technology.
Key Alternatives
While the Immunoassay Analyzer is a leading product in ANA testing, there are other alternatives available, such as manual ELISA kits and semi-automated analyzers. Manual ELISA kits are less expensive but require more manual labor and are prone to errors. Semi-automated analyzers offer some automation but lack the advanced features and performance of the Immunoassay Analyzer.
Expert Overall Verdict & Recommendation
Overall, the Immunoassay Analyzer is a highly effective and reliable tool for ANA testing, offering significant advantages in terms of accuracy, efficiency, and throughput. While it represents a significant investment, the benefits outweigh the costs for laboratories that require high-quality ANA testing services. We recommend the Immunoassay Analyzer for laboratories seeking to improve their ANA testing capabilities and deliver better patient care.
Insightful Q&A Section
- Question: What is the clinical significance of different ANA patterns (e.g., homogeneous, speckled, nucleolar)?
- Question: How does the ANA titer correlate with disease activity in autoimmune diseases?
- Question: What follow-up tests should be ordered after a positive ANA result?
- Question: Can a negative ANA result rule out an autoimmune disease?
- Question: How does the ANA test differ from other antibody tests used to diagnose autoimmune diseases?
- Question: What are the limitations of the ANA test, and how can they be addressed?
- Question: How often should the ANA test be repeated in patients with a history of autoimmune disease?
- Question: What is the role of ANA testing in the diagnosis of drug-induced lupus?
- Question: How does ANA testing differ in children compared to adults?
- Question: What are the emerging trends and advancements in ANA testing technology?
Answer: Different ANA patterns can be associated with specific autoimmune diseases. Homogeneous patterns are often seen in SLE, speckled patterns in MCTD and Sjögren’s syndrome, and nucleolar patterns in systemic sclerosis. However, patterns are not diagnostic on their own and must be interpreted in conjunction with other clinical and laboratory findings.
Answer: While a higher ANA titer generally suggests a greater likelihood of an autoimmune disease, the titer does not always correlate directly with disease activity. Some patients with high titers may have mild symptoms, while others with lower titers may have severe disease. Monitoring specific disease markers and clinical symptoms is more important for assessing disease activity.
Answer: The specific follow-up tests will depend on the clinical context and the suspected autoimmune disease. Common follow-up tests include anti-dsDNA, anti-Smith, anti-Ro (SSA), anti-La (SSB), anti-RNP, anti-Scl-70, and anti-centromere antibodies. Additional tests may be ordered to assess organ involvement and inflammation.
Answer: A negative ANA result makes an autoimmune disease less likely, but it does not completely rule it out. Some patients with autoimmune diseases, particularly those with limited or organ-specific disease, may have negative ANA results. In such cases, other specific antibody tests and clinical criteria are used for diagnosis.
Answer: The ANA test is a screening test that detects the presence of antinuclear antibodies, which are common in many autoimmune diseases. Other antibody tests, such as anti-dsDNA and anti-Smith, are more specific for certain autoimmune diseases, such as SLE. These specific antibody tests are often used to confirm or refine the diagnosis after a positive ANA result.
Answer: The ANA test has limitations, including the potential for false positives and false negatives. False positives can occur due to age, sex, medications, and infections. False negatives can occur in patients with limited or organ-specific disease. These limitations can be addressed by interpreting the ANA result in conjunction with other clinical and laboratory findings and by ordering specific antibody tests as needed.
Answer: The frequency of ANA testing in patients with a history of autoimmune disease depends on the clinical situation. In general, ANA testing is not repeated routinely unless there is a change in symptoms or disease activity. Monitoring specific disease markers and clinical symptoms is more important for assessing disease activity.
Answer: Drug-induced lupus is a lupus-like syndrome that can be caused by certain medications. A positive ANA is common in drug-induced lupus, and the pattern of the ANA may be different from that seen in SLE. The diagnosis of drug-induced lupus is based on clinical criteria, including the temporal relationship between medication exposure and the onset of symptoms, as well as the resolution of symptoms after discontinuation of the medication.
Answer: The interpretation of ANA testing in children is similar to that in adults. However, the prevalence of positive ANA results may be different in children, and certain autoimmune diseases, such as juvenile idiopathic arthritis, are more common in children. Specific antibody tests and clinical criteria are used to diagnose autoimmune diseases in children.
Answer: Emerging trends in ANA testing technology include the development of more sensitive and specific assays, as well as the use of automated platforms to improve efficiency and reduce errors. Multiplex assays that can detect multiple antibodies simultaneously are also being developed. These advancements are expected to improve the accuracy and efficiency of ANA testing and lead to better patient outcomes.
Conclusion & Strategic Call to Action
In conclusion, understanding the nuances of ANA positive results and their corresponding ICD-10 coding is paramount for accurate diagnosis and effective management of autoimmune diseases. This comprehensive guide has provided an in-depth exploration of the ANA test, its significance, the relevant ICD-10 codes, and the common autoimmune conditions associated with positive results. The Immunoassay Analyzer stands as a leading product, enhancing the accuracy and efficiency of ANA testing in modern diagnostic laboratories. By integrating expert insights and practical guidance, we’ve aimed to empower healthcare professionals and patients alike with the knowledge needed to navigate this complex landscape. The future of ANA testing holds promise with emerging technologies and advancements that will further refine diagnostic capabilities.
Now that you have a deeper understanding of ANA positive ICD-10, we encourage you to share your experiences and insights in the comments below. Your contributions can help others navigate this complex topic and foster a collaborative learning environment. For further exploration, explore our advanced guide to autoimmune disease management. If you have specific questions or require personalized guidance, contact our experts for a consultation on ANA positive ICD-10 coding and diagnosis.