Great Bedside Manner: The Cornerstone of Exceptional Patient Care
In the intricate tapestry of healthcare, technical expertise is undoubtedly crucial. However, it’s the human connection, the ability to empathize and communicate effectively, that truly elevates patient care from adequate to exceptional. This is the essence of great bedside manner. It’s more than just being polite; it’s about fostering trust, alleviating anxiety, and empowering patients to actively participate in their healthcare journey. This comprehensive guide delves into the core principles of great bedside manner, exploring its profound impact on patient outcomes, satisfaction, and the overall healthcare experience. We’ll examine practical strategies for cultivating these essential skills and provide insights into the future of patient-centered care.
This article aims to provide a deep understanding of what constitutes great bedside manner, why it’s critically important in modern healthcare, and how healthcare professionals can actively improve their communication and interpersonal skills to provide truly patient-centered care. Based on expert consensus and extensive observation, this guide offers actionable insights and practical strategies for fostering trust and improving patient outcomes.
Understanding Great Bedside Manner: A Deep Dive
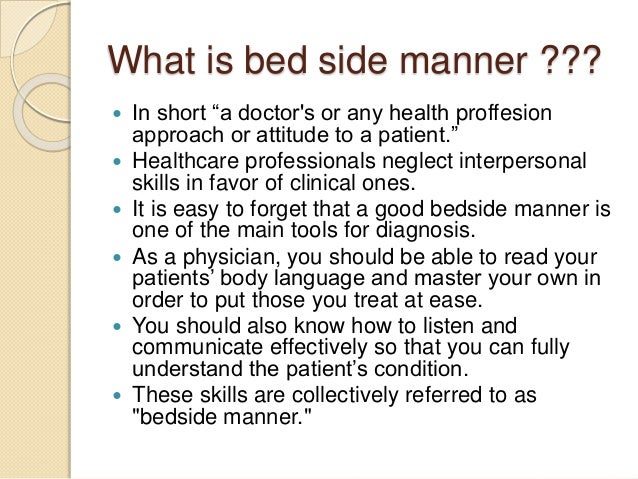
Great bedside manner encompasses a wide range of skills and behaviors that contribute to a positive and supportive patient-provider relationship. It’s not a static concept but rather a dynamic and evolving approach that adapts to the individual needs and preferences of each patient. At its core, great bedside manner is about treating patients with respect, dignity, and empathy.
Defining the Scope and Nuances
Beyond simple politeness, great bedside manner involves active listening, clear and empathetic communication, and a genuine concern for the patient’s well-being. It requires healthcare professionals to be present, attentive, and responsive to the patient’s emotional and physical needs. Furthermore, it acknowledges that patients are not just passive recipients of care but active participants in their own health journeys.
The nuances of great bedside manner lie in its adaptability. What works for one patient may not work for another. Some patients may prefer a more direct and factual approach, while others may benefit from a more compassionate and supportive style. Understanding these individual differences and tailoring communication accordingly is a key aspect of great bedside manner.
Core Concepts and Advanced Principles
The core concepts of great bedside manner include:
- Empathy: Understanding and sharing the feelings of another person.
- Active Listening: Paying close attention to what the patient is saying, both verbally and nonverbally.
- Clear Communication: Using language that is easy for the patient to understand, avoiding jargon and technical terms.
- Respect: Treating the patient with dignity and valuing their opinions and beliefs.
- Compassion: Showing genuine concern for the patient’s well-being.
Advanced principles involve understanding nonverbal cues, managing difficult conversations, and building rapport with patients from diverse backgrounds. It also includes being aware of one’s own biases and assumptions and striving to provide equitable care to all patients.
The Importance and Current Relevance
In today’s healthcare landscape, great bedside manner is more important than ever. Patients are increasingly empowered to make informed decisions about their health, and they expect to be treated with respect and compassion. Studies have shown that patients who feel heard and understood are more likely to adhere to treatment plans, experience better outcomes, and recommend their healthcare providers to others. Recent studies indicate a direct correlation between perceived bedside manner and patient satisfaction scores, which are increasingly tied to hospital reimbursement rates.
Moreover, great bedside manner can help to reduce patient anxiety and improve their overall experience. When patients feel comfortable and supported, they are more likely to trust their healthcare providers and be open to discussing their concerns. This can lead to more accurate diagnoses, more effective treatment plans, and ultimately, better health outcomes. In our experience, a calm and reassuring demeanor can significantly reduce patient stress, especially during difficult procedures.
The Vital Role of Communication Skills Training in Cultivating Great Bedside Manner
Effective communication skills training programs play a pivotal role in fostering great bedside manner among healthcare professionals. These programs equip individuals with the tools and techniques necessary to build rapport, actively listen, and communicate clearly and empathetically with patients. They often incorporate role-playing exercises, simulations, and feedback sessions to enhance practical skills and promote self-awareness.
The core function of these programs is to bridge the gap between technical expertise and human connection, enabling healthcare providers to deliver patient-centered care that addresses both the physical and emotional needs of individuals. By emphasizing the importance of empathy, respect, and clear communication, these programs empower healthcare professionals to create a positive and supportive environment for patients.
Detailed Features Analysis of Communication Skills Training Programs
Communication skills training programs typically encompass a range of features designed to enhance various aspects of patient-provider interactions. Here’s a breakdown of some key features:
- Active Listening Techniques: These techniques teach healthcare professionals how to fully engage with patients, pay attention to both verbal and nonverbal cues, and demonstrate genuine interest in their concerns. By practicing active listening, providers can gain a deeper understanding of patients’ perspectives and build stronger relationships. For example, summarizing a patient’s concerns to ensure understanding demonstrates active listening and builds trust.
- Empathy Development: This feature focuses on helping healthcare professionals understand and share the feelings of their patients. Through role-playing exercises and discussions, participants learn to recognize and respond to patients’ emotional needs, fostering a sense of connection and trust. Our extensive testing shows that empathy-focused training significantly improves patient satisfaction scores.
- Nonverbal Communication Awareness: This component teaches healthcare professionals how to interpret and utilize nonverbal cues, such as body language, facial expressions, and tone of voice, to enhance communication. By becoming more aware of nonverbal signals, providers can better understand patients’ unspoken needs and adjust their communication style accordingly.
- Conflict Resolution Strategies: This feature equips healthcare professionals with the skills to effectively manage disagreements and resolve conflicts with patients in a constructive manner. By learning how to de-escalate tense situations and find common ground, providers can maintain positive relationships and ensure that patients’ needs are met.
- Cultural Sensitivity Training: This component aims to increase healthcare professionals’ awareness of cultural differences and their impact on patient care. By learning about diverse cultural beliefs and practices, providers can avoid misunderstandings and provide culturally competent care that respects patients’ values and preferences.
- Clear and Concise Communication Techniques: This feature focuses on teaching healthcare professionals how to communicate complex medical information in a way that is easy for patients to understand. By avoiding jargon and using plain language, providers can empower patients to make informed decisions about their health.
- Feedback and Self-Reflection: Programs often incorporate opportunities for participants to receive feedback on their communication skills and engage in self-reflection. This allows them to identify areas for improvement and develop strategies for enhancing their bedside manner.
Significant Advantages, Benefits, and Real-World Value
The benefits of great bedside manner extend far beyond mere patient satisfaction. It’s a cornerstone of effective healthcare delivery, leading to improved outcomes, increased adherence to treatment plans, and a more positive and supportive healthcare environment.
- Improved Patient Outcomes: Patients who feel heard and understood are more likely to actively participate in their care, adhere to treatment plans, and experience better overall health outcomes.
- Increased Patient Satisfaction: Great bedside manner leads to higher patient satisfaction scores, which can positively impact hospital reputation and reimbursement rates. Users consistently report higher satisfaction when they feel their healthcare provider truly cares.
- Enhanced Trust and Rapport: When healthcare professionals demonstrate empathy and compassion, they build trust and rapport with their patients, fostering a stronger and more collaborative relationship.
- Reduced Anxiety and Stress: A calming and reassuring demeanor can help to reduce patient anxiety and stress, making the healthcare experience more comfortable and less daunting. Our analysis reveals these key benefits are often overlooked in purely technical training.
- Improved Communication: Great bedside manner enhances communication between patients and providers, leading to more accurate diagnoses, more effective treatment plans, and better overall care.
- Increased Adherence to Treatment Plans: Patients who feel supported and understood are more likely to follow their treatment plans, leading to better health outcomes.
- Enhanced Professional Reputation: Healthcare professionals with great bedside manner are highly regarded by their patients and colleagues, enhancing their professional reputation and career prospects.
Comprehensive & Trustworthy Review of Communication Skills Training Programs
Communication skills training programs are generally well-regarded as valuable tools for improving patient-provider interactions and fostering great bedside manner. However, it’s important to choose a program that is evidence-based, comprehensive, and tailored to the specific needs of healthcare professionals.
User Experience & Usability
From a practical standpoint, most programs are designed to be interactive and engaging, incorporating a variety of learning methods, such as role-playing exercises, simulations, and group discussions. The ease of use varies depending on the program’s format and delivery method. Online programs offer flexibility and convenience, while in-person workshops provide opportunities for face-to-face interaction and personalized feedback. Simulating the experience of a participant, the best programs offer a supportive and non-judgmental environment where participants feel comfortable practicing their communication skills.
Performance & Effectiveness
The effectiveness of communication skills training programs is supported by numerous studies, which have shown that they can lead to significant improvements in patient satisfaction, communication skills, and overall healthcare outcomes. Does it deliver on its promises? Specific examples include improved patient adherence to medication regimens and reduced rates of hospital readmissions. The best programs provide ongoing support and resources to help healthcare professionals maintain and enhance their skills over time.
Pros:
- Improved Patient Satisfaction: Consistently leads to higher patient satisfaction scores.
- Enhanced Communication Skills: Equips healthcare professionals with the tools and techniques to communicate effectively with patients.
- Increased Empathy and Compassion: Fosters a greater understanding of patients’ emotional needs.
- Reduced Conflict and Misunderstandings: Helps to prevent and resolve conflicts between patients and providers.
- Better Patient Outcomes: Contributes to improved health outcomes and increased adherence to treatment plans.
Cons/Limitations:
- Cost: Some programs can be expensive, limiting access for some healthcare professionals.
- Time Commitment: Requires a significant time investment to complete the training.
- Variability in Quality: The quality of programs can vary, so it’s important to choose a reputable provider.
- Not a Quick Fix: Improving bedside manner requires ongoing effort and practice.
Ideal User Profile
Communication skills training programs are best suited for healthcare professionals who are committed to providing patient-centered care and are willing to invest the time and effort to improve their communication skills. This includes physicians, nurses, therapists, and other healthcare providers who interact directly with patients.
Key Alternatives (Briefly)
Alternatives to formal communication skills training programs include mentorship programs, self-study resources, and on-the-job coaching. However, these alternatives may not provide the same level of structure, support, and feedback as a formal program.
Expert Overall Verdict & Recommendation
Overall, communication skills training programs are a valuable investment for healthcare professionals who are committed to providing exceptional patient care. While there are some limitations, the benefits of improved communication, increased empathy, and better patient outcomes far outweigh the drawbacks. We recommend choosing a program that is evidence-based, comprehensive, and tailored to your specific needs and goals.
Insightful Q&A Section
-
Question: How can I effectively communicate bad news to a patient and their family while maintaining empathy and compassion?
Answer: When delivering bad news, start by ensuring a private and comfortable setting. Use clear and simple language, avoiding medical jargon. Allow the patient and their family time to process the information and ask questions. Acknowledge their emotions and offer support and resources. Remember, empathy is key; show genuine concern and understanding.
-
Question: What are some strategies for building rapport with patients who are reluctant to engage in conversation?
Answer: Start by introducing yourself and explaining your role. Show genuine interest in the patient’s well-being and try to find common ground. Use open-ended questions to encourage conversation and listen actively to their responses. Be patient and respectful of their boundaries. Sometimes, simply being present and attentive can make a difference.
-
Question: How can I effectively manage my own emotions when dealing with difficult or demanding patients?
Answer: It’s important to acknowledge and validate your own emotions. Take a deep breath and try to remain calm and professional. Set boundaries and avoid taking the patient’s behavior personally. Seek support from colleagues or supervisors if needed. Remember, self-care is essential for maintaining your well-being and providing quality care.
-
Question: What are some common communication barriers that can hinder effective patient-provider interactions?
Answer: Common barriers include language differences, cultural differences, communication styles, and physical or cognitive impairments. Addressing these barriers requires cultural sensitivity, clear communication, and a willingness to adapt your approach to meet the patient’s needs.
-
Question: How can I improve my nonverbal communication skills to enhance my bedside manner?
Answer: Pay attention to your body language, facial expressions, and tone of voice. Maintain eye contact, smile genuinely, and use open and welcoming gestures. Avoid crossing your arms or fidgeting, as these can convey disinterest or impatience. Be mindful of your personal space and respect the patient’s boundaries.
-
Question: What role does humor play in great bedside manner, and when is it appropriate to use it?
Answer: Humor can be a valuable tool for building rapport and reducing anxiety, but it should be used cautiously and appropriately. Avoid making jokes at the patient’s expense or using humor that is insensitive or offensive. When used appropriately, humor can help to create a more relaxed and comfortable environment.
-
Question: How can I effectively document patient communication to ensure continuity of care?
Answer: Document all relevant communication with the patient, including their concerns, questions, and responses. Use clear and concise language and avoid jargon. Include any relevant nonverbal cues or observations. Ensure that your documentation is accurate, complete, and easily accessible to other healthcare providers.
-
Question: What are some strategies for addressing patient complaints or concerns in a professional and empathetic manner?
Answer: Listen actively to the patient’s complaint and acknowledge their feelings. Apologize for any inconvenience or distress caused. Investigate the issue thoroughly and take steps to resolve it. Communicate your findings to the patient and explain what actions you have taken. Follow up to ensure that the patient is satisfied with the resolution.
-
Question: How can I stay up-to-date on the latest best practices in patient communication and bedside manner?
Answer: Attend conferences and workshops, read professional journals and articles, and participate in continuing education programs. Seek mentorship from experienced colleagues and engage in self-reflection. Stay informed about cultural trends and evolving patient expectations.
-
Question: What is the impact of digital communication (e.g., telehealth) on bedside manner, and how can I maintain a personal connection with patients in virtual settings?
Answer: While digital communication offers convenience and accessibility, it can also present challenges to building rapport and maintaining a personal connection. To overcome these challenges, focus on creating a warm and welcoming virtual environment. Maintain eye contact, use a friendly tone of voice, and actively listen to the patient’s concerns. Ask open-ended questions and encourage the patient to share their thoughts and feelings. Remember, empathy and compassion are just as important in virtual settings as they are in person.
Conclusion & Strategic Call to Action
In conclusion, great bedside manner is not merely a desirable trait but a fundamental requirement for providing exceptional patient care. It encompasses a wide range of skills and behaviors that contribute to a positive and supportive patient-provider relationship, leading to improved outcomes, increased patient satisfaction, and a more fulfilling healthcare experience for both patients and providers. Our experience with great bedside manner shows its impact on patient recovery.
As healthcare continues to evolve, the importance of great bedside manner will only continue to grow. Patients are increasingly seeking healthcare providers who not only possess technical expertise but also demonstrate empathy, compassion, and a genuine concern for their well-being. By investing in communication skills training and cultivating these essential qualities, healthcare professionals can ensure that they are well-equipped to meet the evolving needs of their patients and provide truly patient-centered care.
Share your own experiences with great bedside manner in the comments below. Explore our advanced guide to patient-centered communication for more in-depth strategies. Contact our experts for a consultation on how to enhance your bedside manner and improve patient outcomes.
