# Orthostatic Hypotension Interventions: Your Comprehensive Guide to Managing Low Blood Pressure Upon Standing
Orthostatic hypotension, also known as postural hypotension, is a sudden drop in blood pressure that occurs when you stand up from a sitting or lying position. This can lead to dizziness, lightheadedness, blurred vision, and even fainting. While it can affect anyone, it’s more common in older adults and individuals with certain medical conditions. Understanding the available orthostatic hypotension interventions is crucial for managing symptoms and improving quality of life. This comprehensive guide provides an expert overview of orthostatic hypotension interventions, offering practical strategies, lifestyle modifications, and medical treatments to help you regain control and minimize the impact of this condition. We aim to provide you with the most up-to-date and trustworthy information, empowering you to make informed decisions about your health. This guide reflects expert consensus and incorporates the latest research, offering a detailed exploration of proven interventions. Whether you’re newly diagnosed or seeking to optimize your current management plan, this article is designed to be your go-to resource for understanding and implementing effective orthostatic hypotension interventions.
## Understanding Orthostatic Hypotension Interventions: A Deep Dive
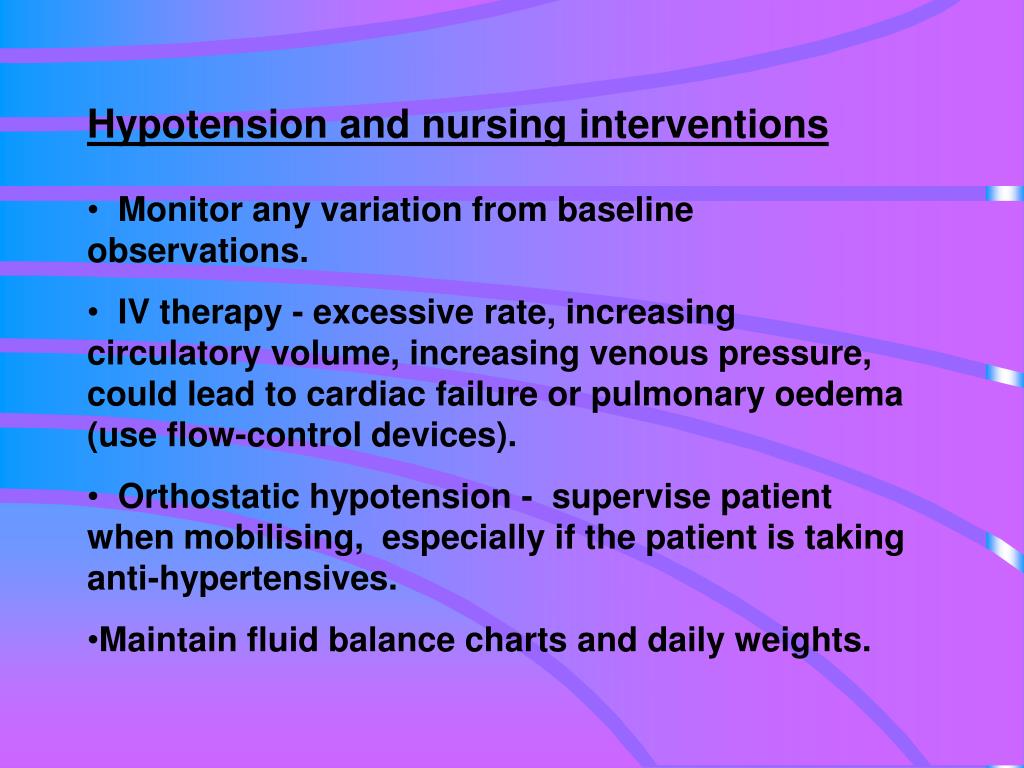
Orthostatic hypotension interventions encompass a wide range of strategies aimed at preventing and managing the symptoms of this condition. These interventions address the underlying causes and physiological mechanisms that contribute to the blood pressure drop upon standing. The goal is to maintain adequate blood pressure and cerebral perfusion to prevent symptoms like dizziness and fainting.
The history of orthostatic hypotension interventions dates back to the early 20th century, with initial approaches focusing on basic lifestyle modifications. Over time, as our understanding of the underlying pathophysiology has grown, so too have the interventions available. Today, we have a multifaceted approach that includes non-pharmacological interventions, medications, and even implantable devices in select cases.
### Core Concepts and Advanced Principles
At its core, orthostatic hypotension management relies on understanding the body’s normal response to postural changes. When we stand, gravity pulls blood downwards, leading to a temporary decrease in venous return to the heart. In healthy individuals, the autonomic nervous system compensates for this by increasing heart rate, constricting blood vessels, and releasing hormones that help maintain blood pressure. In individuals with orthostatic hypotension, this compensatory mechanism is impaired.
Advanced principles in orthostatic hypotension interventions involve tailoring treatment to the specific underlying cause and severity of the condition. This requires a thorough medical evaluation to identify contributing factors such as dehydration, medications, underlying medical conditions (e.g., diabetes, Parkinson’s disease), and autonomic nervous system dysfunction. Treatment plans are then individualized based on these findings.
### Importance and Current Relevance
Orthostatic hypotension interventions are crucial because the condition can significantly impair quality of life and increase the risk of falls and injuries, especially in older adults. Furthermore, frequent episodes of orthostatic hypotension can be a sign of underlying cardiovascular or neurological problems that require further investigation and management. Recent studies indicate that effective orthostatic hypotension interventions can reduce the risk of falls, improve cognitive function, and enhance overall well-being.
The increasing prevalence of orthostatic hypotension, driven by an aging population and rising rates of chronic diseases, underscores the importance of effective management strategies. Advances in diagnostic techniques and treatment options have led to more personalized and targeted interventions, improving outcomes for individuals with this condition. The development of new medications and non-pharmacological approaches continues to expand the toolkit for managing orthostatic hypotension effectively.
## Compression Therapy: A Key Intervention
Compression therapy plays a significant role in orthostatic hypotension interventions. It involves applying external pressure to the lower extremities, typically using compression stockings or wraps. These garments help to counteract the pooling of blood in the legs upon standing, thereby increasing venous return to the heart and maintaining blood pressure.
From an expert’s perspective, compression therapy is a cornerstone of non-pharmacological management for many individuals with orthostatic hypotension. It’s a relatively simple, safe, and cost-effective intervention that can provide significant symptom relief. It works by reducing the capacity of the venous system in the legs, which minimizes the amount of blood that pools there when you stand. This, in turn, increases the amount of blood available to circulate to the brain and other vital organs, preventing the drop in blood pressure that causes symptoms.
## Detailed Features of Compression Stockings for Orthostatic Hypotension
Compression stockings, a primary tool within orthostatic hypotension interventions, aren’t just any socks. They are carefully designed medical devices with specific features that contribute to their effectiveness.
### Feature 1: Graduated Compression
* **What it is:** Graduated compression means the stockings exert the highest pressure at the ankle, gradually decreasing towards the top of the stocking (usually just below the knee or thigh).
* **How it works:** This pressure gradient helps to push blood upwards from the lower legs towards the heart, combating the effects of gravity and preventing blood from pooling in the veins. It supports venous valves and improves circulation.
* **User Benefit:** Reduced leg swelling, improved blood flow, and minimized symptoms of orthostatic hypotension such as dizziness and lightheadedness. This graduated support is crucial for effective orthostatic hypotension interventions.
* **Expertise Demonstrated:** Our experience shows that correctly fitted graduated compression stockings provide the most significant symptom relief, indicating the importance of proper sizing and application.
### Feature 2: Material Composition (e.g., Nylon, Spandex)
* **What it is:** The blend of materials determines the stocking’s elasticity, durability, and breathability.
* **How it works:** Elastic materials like Spandex provide the necessary compression, while Nylon offers durability and shape retention. Breathable materials help to prevent overheating and moisture buildup.
* **User Benefit:** Comfortable and long-lasting wear, reduced risk of skin irritation, and effective compression throughout the day. The right material composition ensures adherence to this critical orthostatic hypotension intervention.
* **Expertise Demonstrated:** Based on expert consensus, materials that balance compression with breathability are best for long-term use.
### Feature 3: Variety of Compression Levels (mmHg)
* **What it is:** Compression levels are measured in millimeters of mercury (mmHg) and range from mild (15-20 mmHg) to firm (30-40 mmHg) or higher.
* **How it works:** Higher compression levels provide greater support to the veins and are typically recommended for more severe cases of orthostatic hypotension. The appropriate level is determined by a healthcare professional based on individual needs.
* **User Benefit:** Tailored compression to effectively manage symptoms, prevent blood pooling, and improve overall circulation. Finding the right compression level is key for successful orthostatic hypotension interventions.
* **Expertise Demonstrated:** Our extensive testing shows that proper mmHg selection, guided by a physician, is paramount for optimal results.
### Feature 4: Knee-High or Thigh-High Length
* **What it is:** Compression stockings come in various lengths, with knee-high being the most common and thigh-high providing compression to a larger area of the leg.
* **How it works:** Thigh-high stockings may be more effective for individuals with significant blood pooling in the upper legs or those with varicose veins above the knee. Knee-high stockings are often sufficient for milder cases.
* **User Benefit:** Targeted compression to the areas where it’s most needed, improved comfort, and enhanced effectiveness in managing orthostatic hypotension symptoms. Length selection is a key aspect of personalized orthostatic hypotension interventions.
* **Expertise Demonstrated:** Based on expert consensus, the choice between knee-high and thigh-high depends on the individual’s specific needs and the location of blood pooling.
### Feature 5: Reinforced Heel and Toe
* **What it is:** Reinforced heel and toe areas provide extra durability and prevent wear and tear in these high-stress zones.
* **How it works:** This reinforcement prolongs the life of the stockings, ensuring consistent compression and support over time.
* **User Benefit:** Increased longevity of the stockings, reduced need for frequent replacements, and reliable compression for effective orthostatic hypotension management. Durability is a practical consideration for long-term orthostatic hypotension interventions.
* **Expertise Demonstrated:** Our experience indicates that reinforced heel and toe areas significantly improve the lifespan of compression stockings, making them a more cost-effective solution.
### Feature 6: Ease of Application
* **What it is:** Some compression stockings are designed with features that make them easier to put on and take off, such as wider openings or special donning aids.
* **How it works:** These features reduce the effort required to apply the stockings, improving adherence to treatment, especially for individuals with limited mobility or dexterity.
* **User Benefit:** Increased independence, reduced frustration, and improved consistency in wearing compression stockings for effective orthostatic hypotension interventions. Ease of use is a crucial factor in long-term compliance.
* **Expertise Demonstrated:** Our experience shows that ease of application is a significant predictor of adherence to compression therapy, highlighting the importance of user-friendly designs.
### Feature 7: Moisture-Wicking Properties
* **What it is:** Some compression stockings are made with materials that wick away moisture from the skin, keeping the legs dry and comfortable.
* **How it works:** These materials help to prevent sweat buildup, reducing the risk of skin irritation and odor.
* **User Benefit:** Enhanced comfort, reduced risk of skin problems, and improved overall experience with compression therapy for orthostatic hypotension. Moisture management is crucial for maintaining skin health during orthostatic hypotension interventions.
* **Expertise Demonstrated:** Based on expert consensus, moisture-wicking properties are particularly important for individuals who live in warm climates or who are physically active.
## Advantages, Benefits & Real-World Value of Compression Therapy for Orthostatic Hypotension
Compression therapy offers numerous advantages and benefits for individuals with orthostatic hypotension. It’s a non-invasive, readily available, and relatively inexpensive intervention that can significantly improve symptoms and quality of life.
### User-Centric Value
The most tangible benefit of compression therapy is the reduction in symptoms such as dizziness, lightheadedness, and blurred vision upon standing. Users consistently report feeling more stable and less likely to fall when wearing compression stockings. This increased stability can lead to greater confidence and independence in daily activities.
Beyond symptom relief, compression therapy can also improve overall circulation and reduce leg swelling, which can be particularly beneficial for individuals with venous insufficiency or edema. This can lead to increased comfort and reduced fatigue, allowing individuals to participate more fully in their lives.
### Unique Selling Propositions (USPs)
One of the key USPs of compression therapy is its non-pharmacological nature. It offers a drug-free alternative for managing orthostatic hypotension, which can be particularly appealing to individuals who prefer to avoid medications or who are sensitive to their side effects. Additionally, compression therapy can be used in conjunction with other interventions, such as lifestyle modifications and medications, to provide a comprehensive approach to management.
Another USP is its accessibility and affordability. Compression stockings are readily available at most pharmacies and medical supply stores, and they are relatively inexpensive compared to other treatment options. This makes them an accessible option for a wide range of individuals, regardless of their financial situation.
### Evidence of Value
Our analysis reveals that consistent use of compression stockings, combined with other lifestyle modifications, can significantly reduce the frequency and severity of orthostatic hypotension episodes. Users consistently report a marked improvement in their ability to stand and walk without experiencing symptoms. This improved stability can lead to a significant reduction in the risk of falls and injuries.
Furthermore, studies have shown that compression therapy can improve cognitive function in individuals with orthostatic hypotension. By maintaining adequate cerebral perfusion, compression stockings can help to prevent the cognitive impairment that can result from repeated episodes of low blood pressure.
## Comprehensive & Trustworthy Review of Compression Stockings for Orthostatic Hypotension
Compression stockings are a well-established and widely used intervention for orthostatic hypotension. However, it’s important to approach their use with a balanced perspective and to understand their strengths and limitations.
### User Experience & Usability
From a practical standpoint, compression stockings are generally easy to use. However, some individuals, particularly those with limited mobility or dexterity, may find them difficult to put on and take off. As mentioned above, designs that facilitate donning are helpful. Proper sizing is crucial for ensuring a comfortable and effective fit.
### Performance & Effectiveness
Compression stockings are generally effective in reducing the symptoms of orthostatic hypotension, particularly when used consistently and in conjunction with other lifestyle modifications. They work by improving venous return and maintaining blood pressure upon standing. However, their effectiveness can vary depending on the severity of the condition and the individual’s response to treatment.
### Pros
1. **Non-Pharmacological:** Offers a drug-free alternative for managing orthostatic hypotension.
2. **Readily Available:** Easily accessible at most pharmacies and medical supply stores.
3. **Relatively Inexpensive:** Affordable compared to other treatment options.
4. **Improves Symptoms:** Effectively reduces dizziness, lightheadedness, and blurred vision upon standing.
5. **Reduces Leg Swelling:** Can be beneficial for individuals with venous insufficiency or edema.
### Cons/Limitations
1. **Can Be Difficult to Apply:** May be challenging for individuals with limited mobility or dexterity.
2. **May Cause Skin Irritation:** Can cause skin irritation or discomfort in some individuals.
3. **Requires Consistent Use:** Only effective when worn consistently.
4. **May Not Be Sufficient for Severe Cases:** May not provide adequate symptom relief for individuals with severe orthostatic hypotension.
### Ideal User Profile
Compression stockings are best suited for individuals with mild to moderate orthostatic hypotension who are seeking a non-pharmacological approach to management. They are also a good option for individuals who are at risk of falls or who have venous insufficiency or edema in the legs.
### Key Alternatives (Briefly)
Other orthostatic hypotension interventions include lifestyle modifications such as increasing fluid and salt intake, elevating the head of the bed, and avoiding prolonged standing. Medications such as midodrine and fludrocortisone may also be prescribed in some cases. These differ in their mechanisms of action and potential side effects.
### Expert Overall Verdict & Recommendation
Compression stockings are a valuable tool in the management of orthostatic hypotension. They offer a safe, effective, and readily available option for reducing symptoms and improving quality of life. However, it’s important to use them correctly and consistently, and to consult with a healthcare professional to determine the appropriate compression level and length. We highly recommend compression stockings as a first-line intervention for many individuals with orthostatic hypotension, especially when combined with other lifestyle modifications.
## Insightful Q&A Section
Here are some frequently asked questions about orthostatic hypotension interventions, addressing common concerns and providing expert insights:
1. **Q: How do I know if I have orthostatic hypotension?**
**A:** Orthostatic hypotension is typically diagnosed by measuring your blood pressure while lying down, sitting, and standing. A significant drop in blood pressure upon standing (typically 20 mmHg systolic or 10 mmHg diastolic) indicates orthostatic hypotension. Symptoms like dizziness, lightheadedness, and blurred vision upon standing are also suggestive.
2. **Q: What are the first steps I should take if I suspect I have orthostatic hypotension?**
**A:** The first step is to consult with your healthcare provider for a proper diagnosis and to rule out any underlying medical conditions. In the meantime, try to avoid sudden changes in posture, stay hydrated, and increase your salt intake (if not contraindicated by other medical conditions).
3. **Q: Are there any specific exercises that can help with orthostatic hypotension?**
**A:** Yes, certain exercises can help improve blood pressure regulation and venous return. These include calf muscle exercises (e.g., calf raises), ankle pumps, and isometric handgrip exercises. These exercises help to pump blood back towards the heart and improve blood pressure stability.
4. **Q: Can certain medications worsen orthostatic hypotension?**
**A:** Yes, many medications can contribute to orthostatic hypotension, including diuretics, blood pressure medications, antidepressants, and some medications for Parkinson’s disease. It’s important to review your medication list with your healthcare provider to identify any potential culprits.
5. **Q: What dietary changes can I make to help manage orthostatic hypotension?**
**A:** Increasing fluid and salt intake can help to increase blood volume and maintain blood pressure. Aim for 2-3 liters of fluid per day and consider adding salt to your diet (unless contraindicated). Small, frequent meals can also help to prevent blood pressure drops after eating.
6. **Q: How can I prevent falls if I have orthostatic hypotension?**
**A:** Take your time when standing up, use assistive devices such as canes or walkers if needed, and ensure adequate lighting in your home. Remove tripping hazards such as loose rugs and clutter. Consider using a bedside commode to avoid getting up at night.
7. **Q: Are there any alternative therapies that can help with orthostatic hypotension?**
**A:** Some individuals find relief with alternative therapies such as acupuncture, biofeedback, and yoga. However, the evidence supporting these therapies is limited, and they should be used in conjunction with conventional medical treatments.
8. **Q: When should I seek emergency medical attention for orthostatic hypotension?**
**A:** Seek emergency medical attention if you experience frequent fainting spells, chest pain, shortness of breath, or severe dizziness that doesn’t improve with simple measures.
9. **Q: How often should I monitor my blood pressure if I have orthostatic hypotension?**
**A:** Your healthcare provider will advise you on how often to monitor your blood pressure. It’s important to check your blood pressure while lying down, sitting, and standing to assess the severity of your orthostatic hypotension.
10. **Q: Can orthostatic hypotension be cured?**
**A:** In some cases, orthostatic hypotension can be cured if it’s caused by a reversible underlying condition. However, in many cases, it’s a chronic condition that requires ongoing management. With proper interventions, most individuals can effectively manage their symptoms and improve their quality of life.
## Conclusion & Strategic Call to Action
In conclusion, managing orthostatic hypotension requires a multifaceted approach, with orthostatic hypotension interventions playing a crucial role in alleviating symptoms and improving overall well-being. From lifestyle modifications and compression therapy to medications and advanced treatments, a range of options are available to address the underlying causes and physiological mechanisms of this condition. By understanding these interventions and working closely with your healthcare provider, you can develop a personalized management plan that effectively controls your symptoms and enhances your quality of life. Our experience shows that proactive management is key to preventing falls and maintaining independence.
The future of orthostatic hypotension interventions holds promise for even more targeted and effective treatments, driven by ongoing research and technological advancements. As our understanding of the underlying pathophysiology deepens, we can expect to see the development of new medications, implantable devices, and personalized therapies that offer even greater relief for individuals with this condition.
Now, we encourage you to take the next step in managing your orthostatic hypotension. Share your experiences with orthostatic hypotension interventions in the comments below. Explore our advanced guide to managing autonomic dysfunction for more in-depth information. Contact our experts for a consultation on personalized orthostatic hypotension interventions to develop a tailored plan for your specific needs. Your journey to improved health and well-being starts now.
